CARDIOVASCULAR JOURNAL OF AFRICA • Vol 23, No 4, May 2012
AFRICA
189
Cardiac troponin I and troponin T are the most specific and
sensitive laboratory markers of myocardial cell injury. However,
they may be elevated in patients presenting with many conditions
other than acute coronary syndrome.
24
Elevated levels of cTnT
were previously considered a specific marker for the diagnosis
of MI. Several recent studies have reported unexpectedly high
cTnT levels in the serum of ICU patients who did not have
underlying coronary syndrome,
9,10,25–28
indicating unrecognised
myocardial injury during their disease process.
It is reasonable to suggest that critically ill patients are at
increased risk of myocardial cell injury. This is due to exposure
to many stresses that increase myocardial oxygen demand,
whereas the myocardial oxygen supply can be limited by
shock, anaemia, tachycardia, hypoxaemia and impaired tissue
perfusion.
9
These events can result in the release of troponin from
cardiomyocytes into the serum. In addition, tumour necrosis
factor (TNF), produced by inflammatory cells, can depress
myocardial function and induce cardiomyocyte apoptosis, which
results in low coronary artery flow and decreased ejection
fraction, which may lead to necrosis and cTnT release from
cardiomyocytes.
29,30
It was found that patients with higher cTnT
levels had a shorter survival rate.
The APACHE II scoring system predominately evaluates
haemodynamic changes rather than heart function, but cTnT
levels could provide a direct marker for cardiac injury, even
if clinically unrecognised. In the present study, the APACHE
II score on ICU admission was significantly different between
patients with elevated and normal cTnT levels. This could have
been due to a more serious baseline condition.
Levels of cTnT on admission and on the seventh day could
predict an adverse prognosis in critically ill patients, whereas
troponin levels on the fourth and 10th days could not. The
peak concentration of cTnT was different in these two groups
(fourth day in surviving patients and seventh day in patients who
died), which in addition to the other findings, represents some
undefined importance in the time of assessment of cTnT levels.
Although serial measurements did not provide additional
statistical value for risk stratification, the different peaks of
troponin levels in deceased and discharged patients are shown in
Fig. 2. Different outcomes during ICU stay related to decreasing
or increasing cTnT levels have not been reported before. We
found that whenever cTnT levels begin to decrease, an adverse
outcome could be expected, and increasing cTnT level was a
predictor of a favourable outcome. This indicates the significant
role that daily changes in cTnT levels play, independent of
baseline cTnT levels.
Ammann
et al
.
17
showed that troponin positivity on admission
was associated with a fourfold increased risk of mortality in 58
critically ill patients without acute coronary syndrome. In their
study, a significant difference in survival between troponin-
positive and troponin-negative patients was found mainly in
a subgroup of patients without volume-refractory shock. This
implied that the analysis of troponin level could predict mortality
in the early but not the late stage of the disease. In another
study by Vlad
et al
., high levels of cTnT on admission had an
independent association with in-hospital, short- and long-term
mortality in 2 078 patients with acute respiratory distress.
31
A limitation of the study was that we did not measure renal
function in any patient. Renal function is an important factor
in cTnT concentrations because the kidney filters cTnT from
the blood. An investigation with a larger sample size is also
necessary. An inevitable limitation of the sample size was
the decreasing number of patients over time because of the
death of some between admission and the 10th day. Another
limitation was the assay method, which could not detect a cTnT
concentration less than 0.01
µ
g/l, so we did not have exact
concentrations for many patients, who were reported to have zero
cTnT concentrations.
Conclusion
We found that levels of cTnT could predict outcome in critically
ill patients at specific times. There was a significant association
between outcome and cTnT level on the first and seventh days
of ICU stay, and a non-significant association with cTnT level on
the fourth and 10th days. The level of cTnT had an association
with outcome and survival, and was shown to be a predictor of
outcome. Cardiac TnT levels during ICU stay did not show a
significant trend overall, which may have been due to the small
sample size (power: 0.26) but changes in cTnT levels at specific
times could be a useful predictor. A study focusing on defining
the best time for measurement of cTnT levels would also provide
crucial data.
References
1.
Robert E., Fromm Jr. Cardiac troponins in the intensive care unit:
Common causes of increased levels and interpretation.
Crit Care Med
2007;
35
(2): 584–588.
2.
Wu AH. Increased troponin in patients with sepsis and septic shock:
myocardial necrosis or reversible myocardial depression?
Intensive
Care Med
2001;
27
: 959–961.
3.
Parker MM. Myocardial dysfunction in sepsis: injury or depression?
Crit Care Med
1999;
27
: 2035–2036.
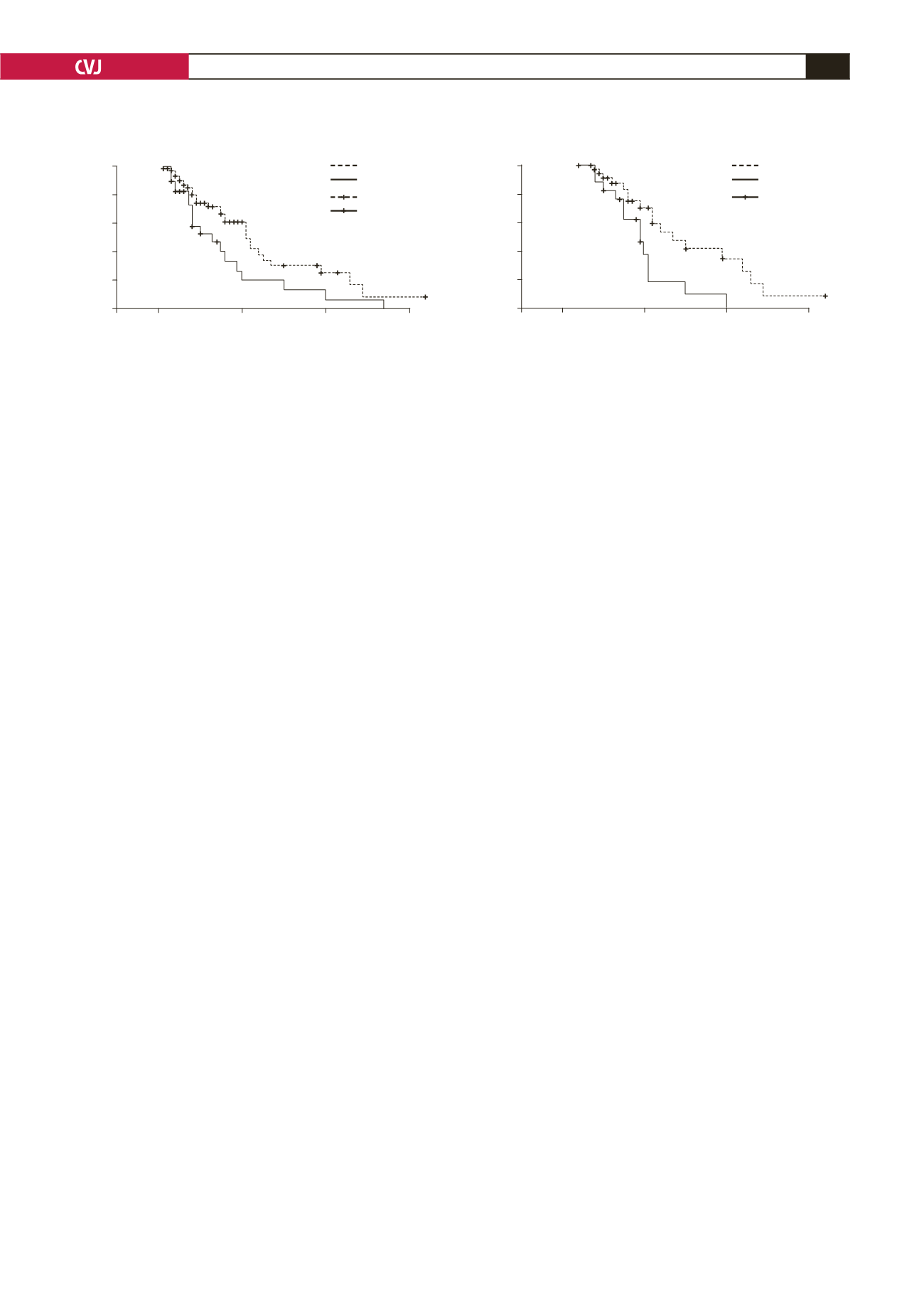
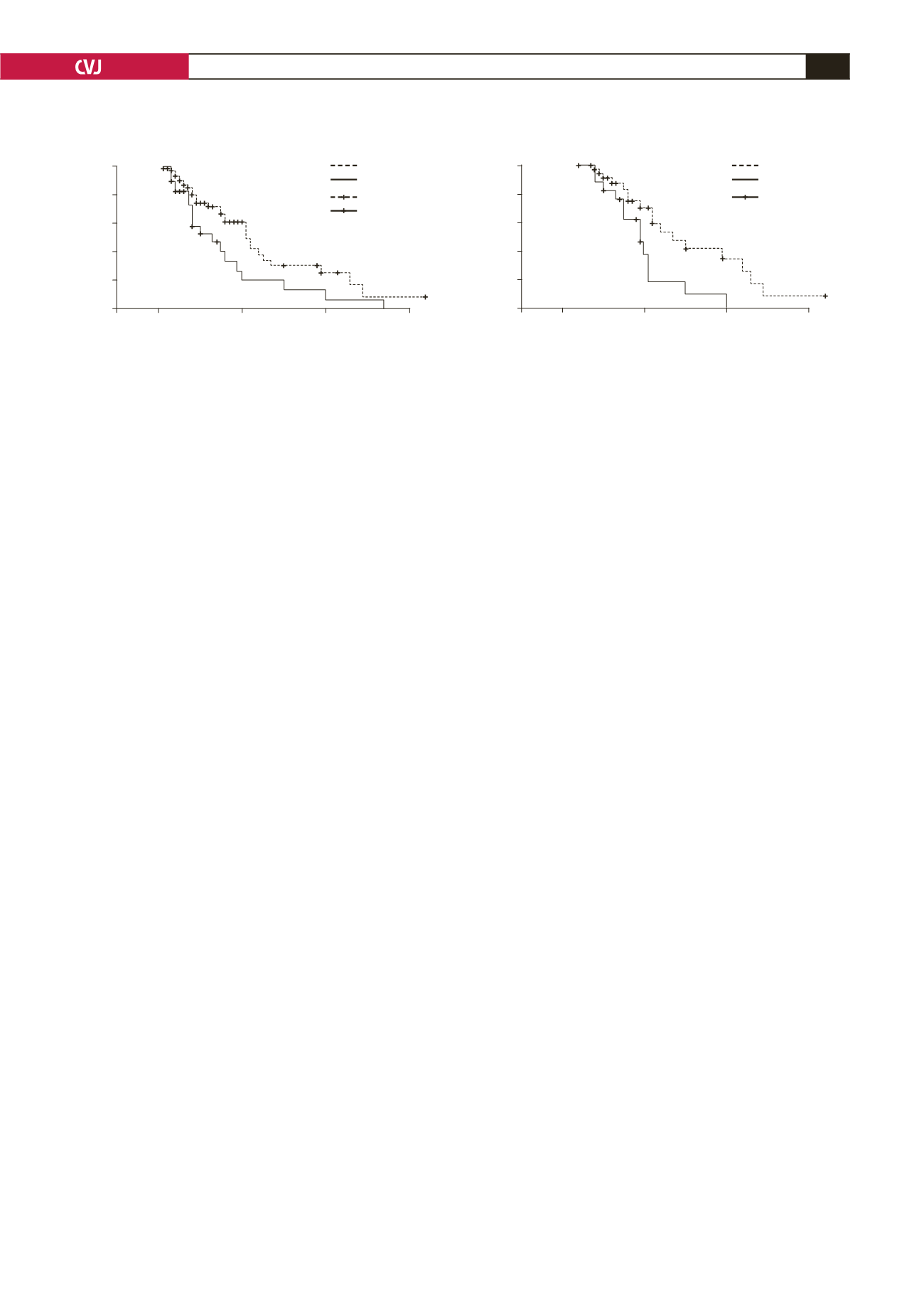
Fig. 3. Patient survival and comparison between patients with high and low cTnT levels on (A) first day of admission
(
p
=
0.027), (B) seventh day of ICU stay (
p
=
0.012).
1.0
0.8
0.6
0.4
0.2
0.0
Cum survival
0
20
40
60
Length of hospital stay (days)
1.0
0.8
0.6
0.4
0.2
0.0
Cum survival
0
30
40
60
Length of hospital stay (days)
< 0.1
> 0.1
< 0.1-censored
> 0.1-censored
cTnT < 0.1
cTnT > 0.1
censored
A
B