S58
AFRICA
CVJAFRICA • Volume 26, No 2, H3Africa Supplement, March/April 2015
This overall lack of prioritisation highlights the need for
improved awareness, understanding and focus, particularly if we
are to unlock the potential that exists for discovering endothelial
targets that could significantly impact on CVD mortality rates.
On this point, it is interesting that there is heterogeneity in
response to metabolic, behavioural and social drivers for CVD.
What if we could understand why some individuals succumb
to CVD risk factors while others don’t? Why do we observe
precocious CVD development in some subgroups exposed to
the same drivers as the rest of a population? Why are there
pockets of positive or negative deviance
27,28
in CVD prevalence
and outcomes within populations exposed to the same socio-
ecological and bio-behavioural risk factors and drivers?
Unlocking the mysteries behind these puzzling differential
responses may rest on targeted efforts to understand the
complicated interplay between known disease drivers and the
genomic and epigenetic mechanisms that underpin pathways of
eNOS uncoupling. Such enlightenment could shape strategies for
addressing the burden of CVD in sub-Saharan Africa and other
regions of the world.
The above notion is paramount, given the prospect of
finding a robust proximal target(s) that can transform our
approach to CVD prevention and treatment, and therefore
should prompt us to reconsider the current status quo regarding
our scientific investments. Insight from the Emerging Risk
factor Collaboration study indicates that we have to screen 400
to 500 people to prevent one CVD event over a period of 10
years.
29
Such modest clinical benefits despite significant financial
investments foster the increasing drum beat from camps that
question the likelihood of meaningful clinical benefit from
identifying and measuring biomarkers.
As a matter of fact, due to the vagaries of causality, some
schools of thought now argue for fewer risk factors instead
of more. Furthermore, although the search for independent
risk factors in medical research has become necessary for the
formulation of risk-stratification schemes, causality cannot be
definitively ascertained, even in controlled clinical trials.
30
In this context, we are beginning to learn that Mendelian
randomisation studies can assess whether risk-factor associations
are truly causal, or due to confounding or reverse causation. An
illustrative NHLBI (National Heart, Lung, and Blood Institute)
example of this is the large-scale Mendelian randomisation study
of high-density lipoprotein (HDL) and the risk of myocardial
infarction (MI), where the investigators found that low-density
lipoprotein (LDL) is likely to be causally related to MI, whereas
HDL is probably only a correlate.
31
This may explain why
LDL-lowering drugs (e.g. statins) reduce risk, whereas every
large trial of HDL-increasing drugs has failed, including the
NHLBI-funded AIM-HIGH trial.
32
Tools such as Mendelian randomisation could help us
make better strategic decisions about drug development, risk
stratification and prediction when deployed via large-scale cohort
studies to identify candidate undiscovered biological pathways
(e.g. endothelial dysfunction) and insights into distinguishing
causality versus correlation. However, the application of such
tools to decipher robust genetic lynchpins of endothelial
dysfunction will require interdisciplinary collaboration and
demand for paradigms that can transform CVD prevention and
treatment efforts.
33
In this context, the H3Africa programme
constitutes a platform to engender collaboration and employ
synergy in intellectual enterprise to address novel research
questions that will inform strategies for CVDdiagnosis, treatment
and prevention in sub-Saharan Africa.
Conclusions
Over the past half century, CVD mortality has declined
appreciably in developed countries, largely secondary to the
risk-factor paradigm that implicated hypertension, cholesterol
and smoking in the genesis of CVD. This risk-factor model led
to targeted research, prevention and treatment efforts to combat
these culprits. More recently, the modulation of inflammation
has presented a unifying framework for achieving further
substantive decline in CVD mortality rates.
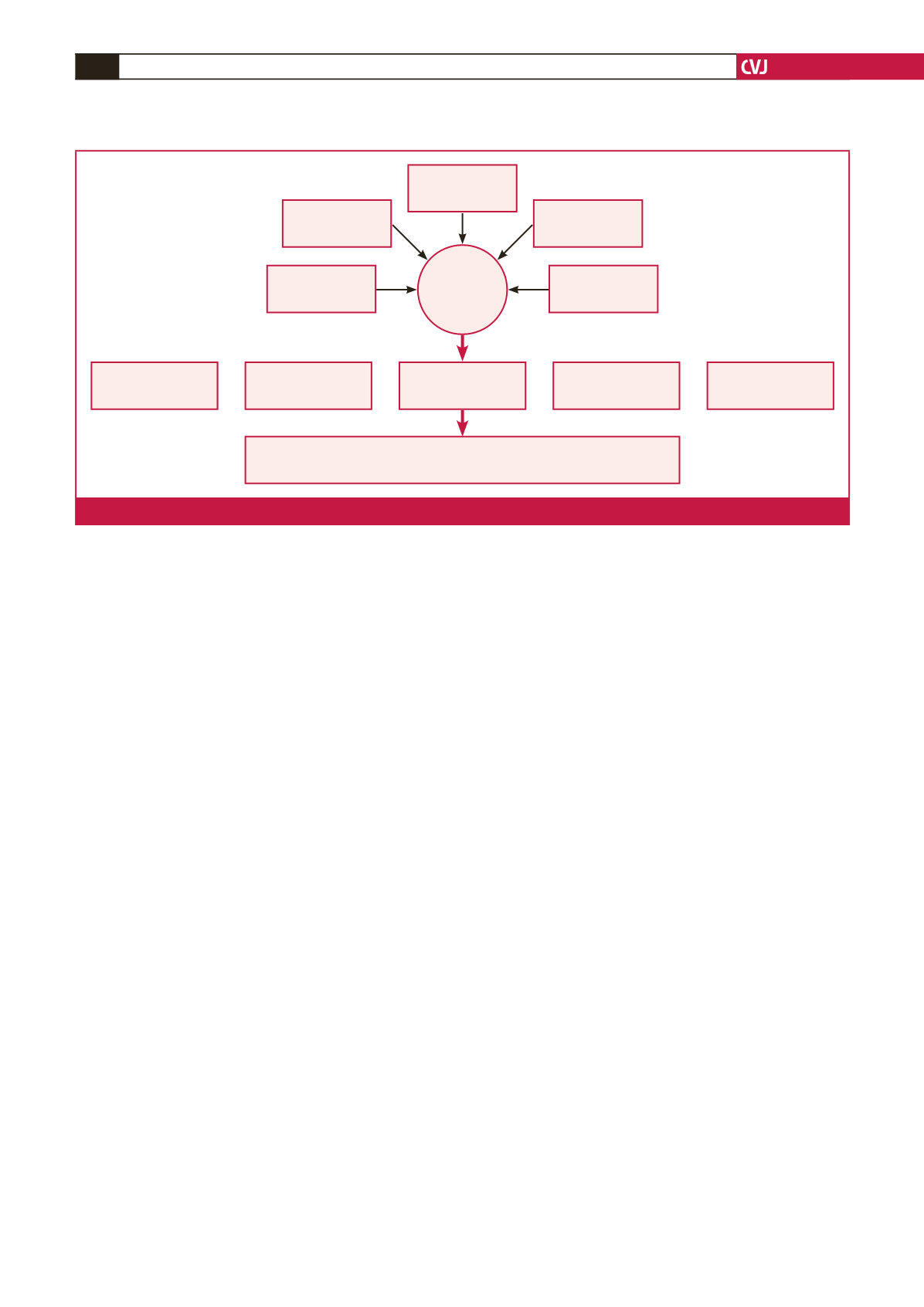
Vascular
remodeling
Atherosclerosis
Inflammation
Thrombosis
Plaque rupture
Contiguous and distant vascular beds involving various organ systems:
Vast spatial distribution, heterogeneity, and complexity
Endothelial
dysfunction
Non-traditional
risk factors
Local
factors
Unknown
factors
Traditional
risk factors
Genetic
factors
Fig. 1.
The endothelium at the Center of Vascular Disease.



















