CARDIOVASCULAR JOURNAL OF AFRICA • Volume 26, No 3, May/June 2015
AFRICA
e9
of cardiac tumours. In this patient it was the transthoracic
echocardiogram at six weeks, followed by the CT scan that
suggested a malignant cause for the pericardial effusion.
Pericardial fluid cytology is unreliable and is not diagnostic in
the majority of patients. Pericardial or endomyocardial biopsy
will be diagnostic in 23 to 50% of samples.
11
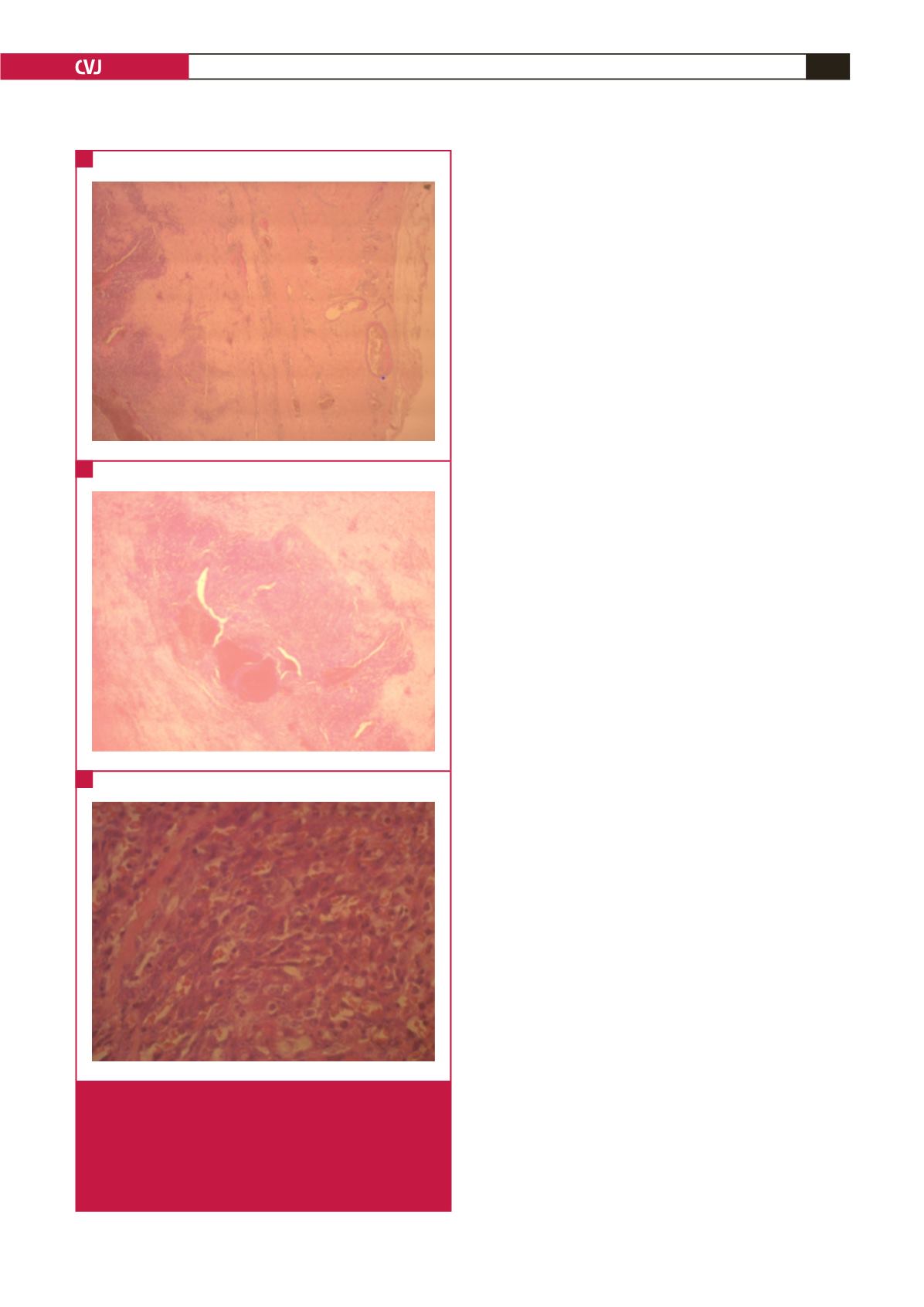
The microscopy of
cardiac angiosarcoma is characterised by anastomotic vascular
channels formed by malignant cells, solid areas of spindle cells
and areas of anaplastic cells. This patient’s biopsy specimens
showed the typical histological features.
This case illustrates the challenges of making a definitive
diagnosis of TB pericarditis in resource-poor settings and that
clinical index can be found wanting when faced with alternative
pathology, as in this patient.
The definitive diagnosis of TB pericarditis is known to be
challenging. The symptoms, chest pain, shortness of breath, fever
and night sweats, are not specific. The signs of a large effusion
include a small-volume pulse, raised jugular venous pulsations,
diffuse apex beat, muffled heart sounds and hepatomegaly. The
presence of fever and a supraclavicular lymph node makes TB
a most probable cause of the effusion. Chest X-ray, ECG and
echocardiography are not specific for TB. There are other causes
of fibrinous pericardial effusions, such as viral and bacterial
infections, uraemia and malignancy.
The definitive diagnosis hinges on finding mycobacteria on
pericardial fluid microscopy or culture as well as histological
examination of a pericardial biopsy. Finding mycobacteria in
other specimens, such as sputum, gastric washings and pleural
fluid in a patient with a fibrinous pericardial effusion makes TB
the most likely cause of the effusion.
12
However, direct smear is only positive in 0–42% of cases of
TB pericarditis. Conventional culture is positive in up to 53% and
this can be improved if direct culture onto liquid Kirchner culture
medium is done. The rate of positive culture goes up to 75%.
In resource-poor settings, microbiology services are limited
so both direct smear and culture are not always available. The
other problem with TB culture is the long delay in getting the
results and for a condition where immediate therapy is needed,
treatment is usually commenced before these results are available.
Pericardial biopsy is invasive and requires the expertise of
a surgeon and this is not usually available where TB is most
common. Pericardial biopsy is diagnostic in 10–64% of cases.
7
Other methods to make a diagnosis of probable pericardial
TB include finding a lymphocyte predominance and a high
protein level in the fluid, clinical index (Tygerberg score), PCR
and indirect tests such as ADA, lysozyme and IFN gamma. The
Tygerberg score comprises weight loss
=
1, night sweats
=
1, fever
of
≥
38°C
=
2, peripheral white cell count
<
10 cells/
μ
l
=
3, and
serum globulin
>
40 g/l
=
3. A total score
≥
6 has a sensitivity of
86% and a specificity of 85%. This is a reasonable approach in a
resource-poor setting.
PCR tends to be expensive, unavailable, and has a high rate
of false-positive results. Adenine deaminase
>
40 IU/l has a
sensitivity of 87% and a specificity of 83%, IFN gamma
>
50 pg/l
has a sensitivity of 92% and specificity of 100% and lysozyme
>
6.6
μ
g/dl has 100% sensitivity and 91% specificity. These three
tests are very good but cost and availability are the limiting
factors in sub-Saharan Africa where TB is very common.
This patient had a low ADA of 24 IU/l; an ADA of
>
35 IU/l
has a sensitivity of
>
95%.
13
The low ADA should have been
Fig. 2.
(A) Pericardium (x 4). Micrograph shows thickened and
fibrosed pericardium with a cellular spindle cell proliferation.
(B) Pericardium (x 20). Photomicrograph shows a nodular
and cellular spindle cell proliferation with large pools of blood.
(C) Pericardium (x 40). Micrograph shows a sieve-like pattern
with spindle cells forming vascular spaces in which there is
red blood cell extravasation.
A
C
B

















