CARDIOVASCULAR JOURNAL OF AFRICA • Volume 26, No 3, May/June 2015
AFRICA
105
and The Guide for the Care and Use of Laboratory Animals.
In addition, the study was conducted with the approval of the
ethics committee.
Two groups were created; the MMF group: group 1 (donors
=
10, recipients
=
10) and the MP group: group 2 (donors
=
nine,
recipients
=
nine). Weights of the rabbits in the MMF group
varied between 2 550 and 3 200 g, whereas the weights in the
MP group varied between 2 560 and 3 150 g. The two groups
were divided into two subgroups, donor and recipient, for
retroperitoneal heterotopic heart transplantation.
The subjects of the MP recipient group received 10 mg/kg/day
methylprednisolone intramuscularly for two days prior to the surgery
(except for the day of surgery). Subjects of the MMF recipient group
received 12.5 mg/kg/day orally via the gavage method for two days
prior to the surgery (except for the day of surgery).
Intramuscular ketamine hydrochloride (50 mg/kg) (Ketalar
®
,
Phizer) and xylazine (10 mg/kg) (Xylazinbio
®
2%, Bioveta) were
administered to the animals. The dose was repeated as a cocktail
containing ketamine (25 mg/kg) and xylazine (5 mg/kg) when
necessary. After anaesthesia, the animals were left to breathe
spontaneously and were provided with nasal oxygen (O
2
) support
at a dose of 2 l/min.
An intravenous catheter (24-gauge) was placed in each
recipient through the marginal ear vein. Over the course of the
procedure, 0.9% sodium chloride (NaCl) solution was infused at
a speed of 4 ml/kg/hour. A catheter (22-gauge) was placed into
the ear artery to monitor blood pressure. The anterior thoracic
area and anterior abdominal wall of the recipient was shaved,
electrocardiography was performed with electrodes placed on
the anterior thoracic wall, and blood pressure was monitored by
connecting the catheter placed into the ear artery to the pressure
transducer (Mennen Medical Inc, Mercury, Revohot, Israel).
The recipient was continuously monitored during abdominal
exploration before the retroperitoneal heterotopic heart
transplantation,duringtransplantation,andaftertransplantation.
Systolic and diastolic blood pressures of the recipients in both
groups were kept at the same level as pre-operative measurements.
Positive inotropic support was provided as required.
The recipient was placed on the operation table in a supine
position. We planned to monitor the recipients for a maximum
of four hours and then sacrifice. The abdomen was accessed
through a median abdominal incision after monitoring and
stabilising the recipients. The retroperitoneum was opened and
the inferior vena cava and abdominal aorta were exposed. These
two vascular configurations were explored and reversed with the
use of tapes. Anticoagulation was provided with 100 U/kg of
standard heparin (Nevparin
®
, Mustafa, Nevzat).
Meanwhile, the donor subject was stabilised in a supine position
and anticoagulationwas providedwith 100U/kg of standardheparin.
After sternotomy the donor heart was excised and crystalloid
cardioplegia was administered through the aortic root. Four mini
vascular clamps were placed in the recipient’s abdominal aorta and
inferior vena cava to prevent blood flow to the anastomoses.
Cold Hospira’s cardioplegia solution (Plegysol
®
, Meditera)
was given through the ascending aorta of the donor’s heart
according to the weight of the donor and at the appropriate
pressure as soon as the vascular configurations were cut. The
time between cutting the ascending aorta of the donor heart and
administration of cardioplegia did not exceed 30 seconds in any
of the groups. Cardioplegia pressure was kept at 15 mmHg.
After the heart became plegic, the superior vena cava (SVC),
inferior vena cava (IVC), and the left atrium were ligatured. The
total duration of ischaemia was between 30 and 35 minutes in
all subjects, and the second cold crystalloid cardioplegia was
administered at the 20th minute. The target was perfusion of the
whole heart and passive working of the left heart, whereas the
working right heart was filled with blood.
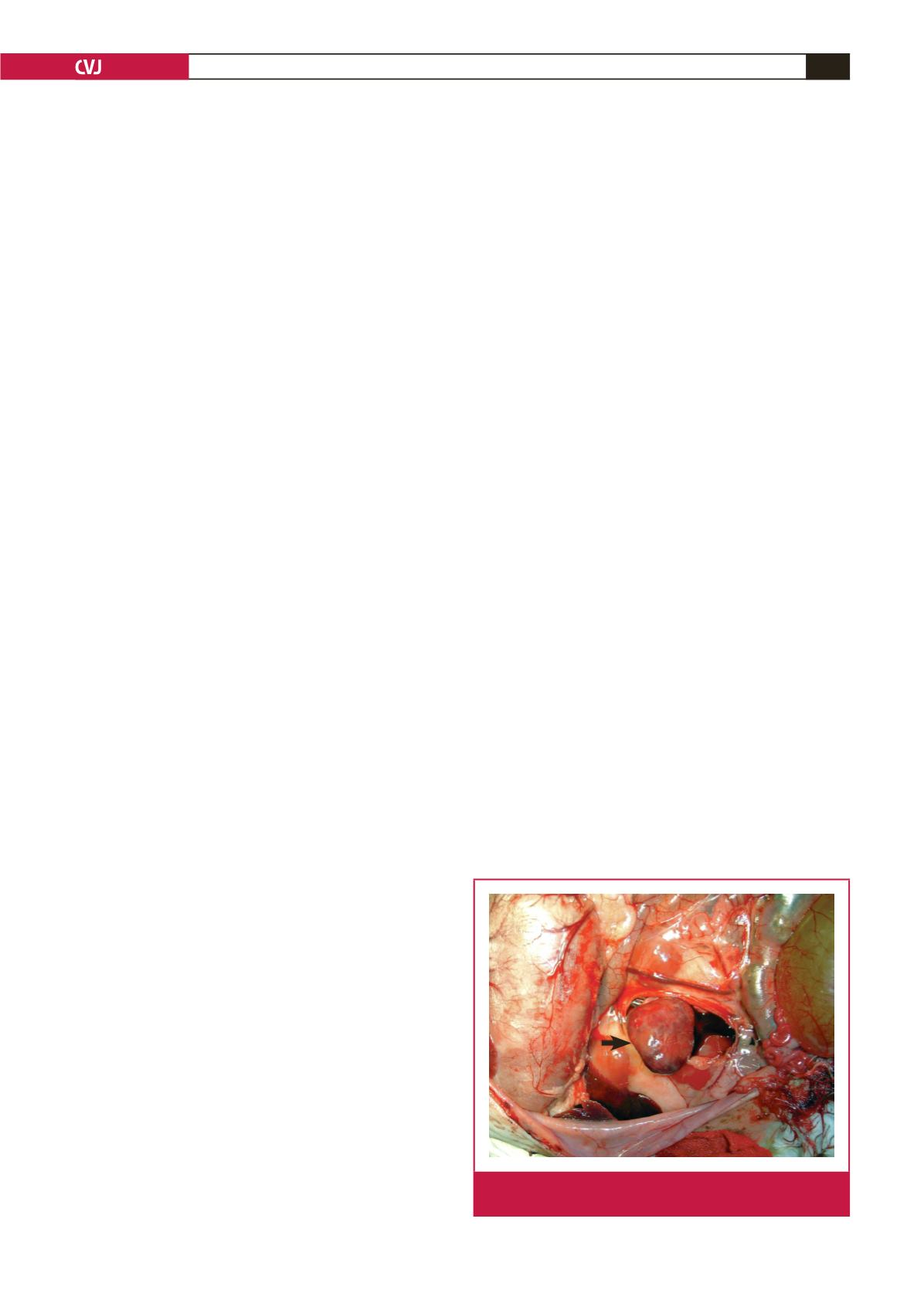
Anastomosis was performed between the ascending aorta
of the transplant and the abdominal aorta of the recipient,
and between the pulmonary artery of the transplant and
the IVC of the recipient. Anastomosis was performed using
7/0 polypropylene suturing material. After transplantation,
the vascular clamps in the abdominal aorta and the IVC of
the recipient were removed (Fig. 1). The transplant worked
spontaneously in sinus rhythm in all experimental groups.
Theheart,whichwastakenfromthedonorandretroperitoneally
implanted in the recipient, functioned for between 2.5 and four
hours in all subjects. Systolic and diastolic blood pressures of
the recipients were kept the same as pre-operative values as far
as possible. Dopamine hydrochloride (Dopamine
®
, Fresenius)
and dobutamine (Dobutabag
®
, Baxter) were used as positive
inotropic support and isotonic 0.9% NaCl solution was used for
fluid replacement. After the abdominal aorta and IVC of the
recipient were clamped, the heart implanted in the recipient was
excised from the anastomosis lines when it stopped functioning.
All recipient subjects were sacrificed at the end of a minimum
of 2.5 hours and a maximum of four hours after the activity of
the transplant had stopped, and the transplant was removed.
Sacrificing was performed using 10% intracardiac formaldehyde
after ketamine (50 mg/kg) and xylazine (10 mg/kg) administration
via the intramuscular route.
Histopathological evaluation
The excised transplant was put into 10% neutral formaldehyde
solution and stored until examination. Sections were made of
the endocardium and myocardium of the right ventricle. After
staining with haematoxylin and eosin, the pathologist from
the Department of Pathology, SUM Faculty of Medicine, who
was blinded to the groups, examined four different areas under
Fig. 1.
The heart was transplanted into the retroperitoneal
area (arrow).

















