CARDIOVASCULAR JOURNAL OF AFRICA • Volume 30, No 1, January/February 2019
AFRICA
53
University ethics review committee. Data used in this study were
obtained from patient charts routinely collected at the clinic, and
a written informed consent was provided before screening by
each participant while attending the HIV clinic. Confidentiality,
anonymity and privacy of all participants were guaranteed at
all levels of this study by excluding all unique identifiers for the
participants.
Baseline assessment included demographic variables, risk
factors for CVD and measurement of body mass index (BMI),
blood pressure, non-fasting total cholesterol and random blood
glucose levels. World Health Organisation (WHO) cardiovascular
risk score was calculated for patients aged above 40 years
8
and
the information included in the patients’ medical record files. All
people with HIV attending the Ukwala HIV clinic were included.
Those who declined consent for the cardiovascular risk-factor
screening and pregnant women were excluded.
Patients fulfilling national eligibility criteria (CD4 count
>
350
cells/mm
3
at time of the study) were treated with standard ART
according to national guidelines.
9
Standard regimens at that
time included tenofovir, lamivudine and efavirenz (TNF/3TC/
EFV) or zidovudine, lamivudine and efavirenz (AZT/3TC/EFV).
Some were still receiving stavudine, lamivudine and efavirenz
(D4T/3TC/EFV), which was being phased out at the time.
A minority received a lopinavir/ritonavir (LPV/r)-containing
regimen.
Prior to commencing CVD screening within the HIV clinics
at Ukwala sub-county hospital, healthcare providers (including
nurses, laboratory technologists, clinicians and data clerks) in the
health facility received a two-day training, followed by regular
intensive theoretical and practical skills training and mentoring
in measuring and interpreting cardiovascular risk factors. The
facility was also provided with regularly calibrated point-of-care
diagnostic equipment for cardiovascular risk assessment.
Blood pressure (BP) was measured using a hospital-grade
Omron M3
®
(Omron, Netherlands) digital automatic blood
pressure machine. Hypertension diagnosis was based on
standard guidelines, and included blood pressure measurements,
medical history, physical examination, assessment of absolute
cardiovascular risks (where deemed necessary by the examining
physician) and laboratory investigations. A comprehensive
assessment of BP involved multiple measurements taken on
separate occasions, at least twice or three times, one or more
weeks apart or sooner if the hypertension was severe.
Hypertension was defined as per the seventh report of the
Joint National Committee on Prevention, Detection, Evaluation
and Treatment of High Blood Pressure (JNC 7)
10
as follows:
pre-hypertension: systolic 120–139 mmHg, diastolic 80–89 mmHg;
stage 1 hypertension: systolic 140–159 mmHg, diastolic 90–99
mmHg; stage 2 hypertension: systolic
≥
160 mmHg, diastolic
≥
100
mmHg, and those currently on antihypertensive drugs.
Total cholesterol and blood glucose levels were measured in
the clinic using finger-prick blood by a Humansence
®
(Human,
Wiesbaden, Germany) meter calibrated with a control strip on the
first and after every 10th specimen. Raised total cholesterol level
was defined according to US National Cholesterol Education
Program ATP III guidelines.
11
Data collection involved the extraction of data from the
patients’ charts using a standardised data tool by trained data
clerks. Charts for patients who attended the clinic from June
2013 to January 2015 were targeted. Those with missing details
on key variables such as cardiovascular risk-factor screening
results and ART regimen were excluded from the data.
Detailed abstraction was then conducted on the remaining
patients’ charts using a data tool that was made up of four
sections, including: (1) anthropometric measures (age, body mass
index, waist circumference and blood pressure), (2) behavioural
and biomedical cardiovascular risk factors (including smoking
status, excessive use of alcohol and non-fasting total cholesterol
level), (3) clinical information (such as on HIV infection and
HIV treatment, ART regimen and duration), and (4) medical
history. Data extracted were entered in a paper data tool then
later transferred into an EpiData software version 3.1 for clean-
up in readiness for analysis using SPSS software.
Statistical analysis
Statistical analysis was performed using SPSS software version
22 (IBM SPSS Statistics, Armonk, NY: IBM Corp). Descriptive
statistics involved calculating the median and interquartile range
(IQR) for continuous data and proportions for categorical
variables. Comparisons of median duration between groups
were done using the Mann–Whitney test with a 5% level
of significance. Associations were assessed using a logistic
regression model, and crude and adjusted odds ratios are
reported with their corresponding confidence intervals.
Results
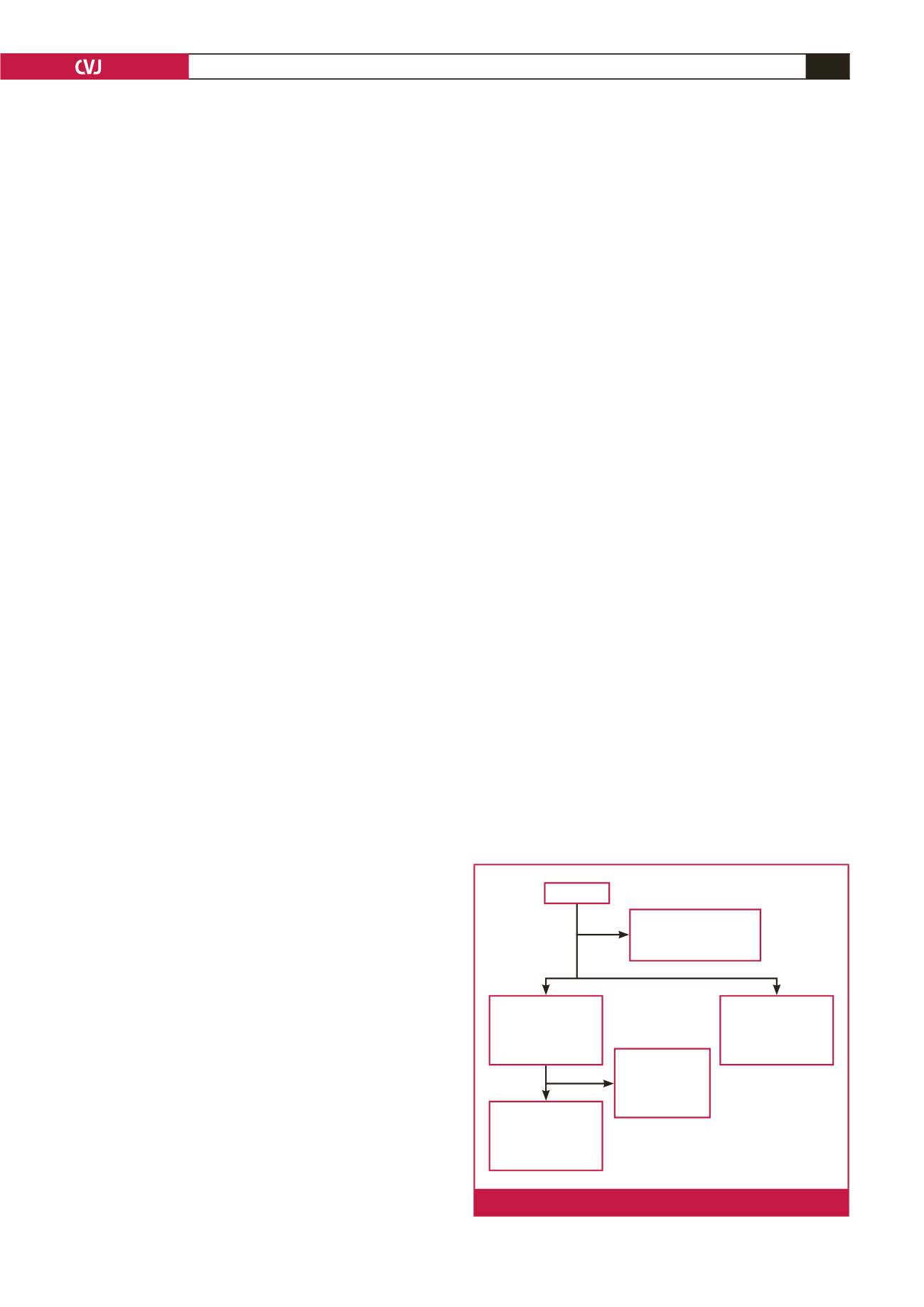
A total of 1 510 subjects was screened, of whom eight were
excluded from analysis because of incomplete data (Fig. 1). Data
collected included demographic variables, risk factors for CVD
and determination of BMI, measurement of blood pressure, and
non-fasting total cholesterol and random blood glucose levels.
Cardiovascular risk score was calculated for those above 40 years
using the WHO (Afri-E) risk-screening chart.
8
Of the subjects screened, 69% (1 036) were women. The
median age was 30 (IQR 31–48) years and median CD4 count
was 430 (IQR 308–574) cells/mm
3
; 79% of subjects were on ART
with a documented regimen. Current smokers were 1.9% (29),
n
=
1 510
n
=
8
with incomplete initial
CVD screening
n
=
1 217
On ART
at initial CVD
screening
n
=
1 181
with complete
information on
ART regimen
n
=
36
Missing
information on
ART regimen
n
=
285
Pre-ART
Had not yet started
ART at initial CVD
screening
Fig. 1.
Data flow chart for cardiovascular risk screening.

















