CARDIOVASCULAR JOURNAL OF AFRICA • Vol 22, No 6, November/December 2011
AFRICA
341
No hepatomegaly or oedema were found.
Haematological parameters and serum biochemistry were
normal. The INR was not available at this time. A 12-lead ECG
revealed a sinus rhythm, with a heart rate of 100 beats/min, mean
frontal QRS axis of +75 and signs of left atrial enlargement. A
chest X-ray showed status pos implantation of a mechanical
prosthesis in the mitral position, pulmonary interstitial oedema,
and cephalisation of the pulmonary vasculature.
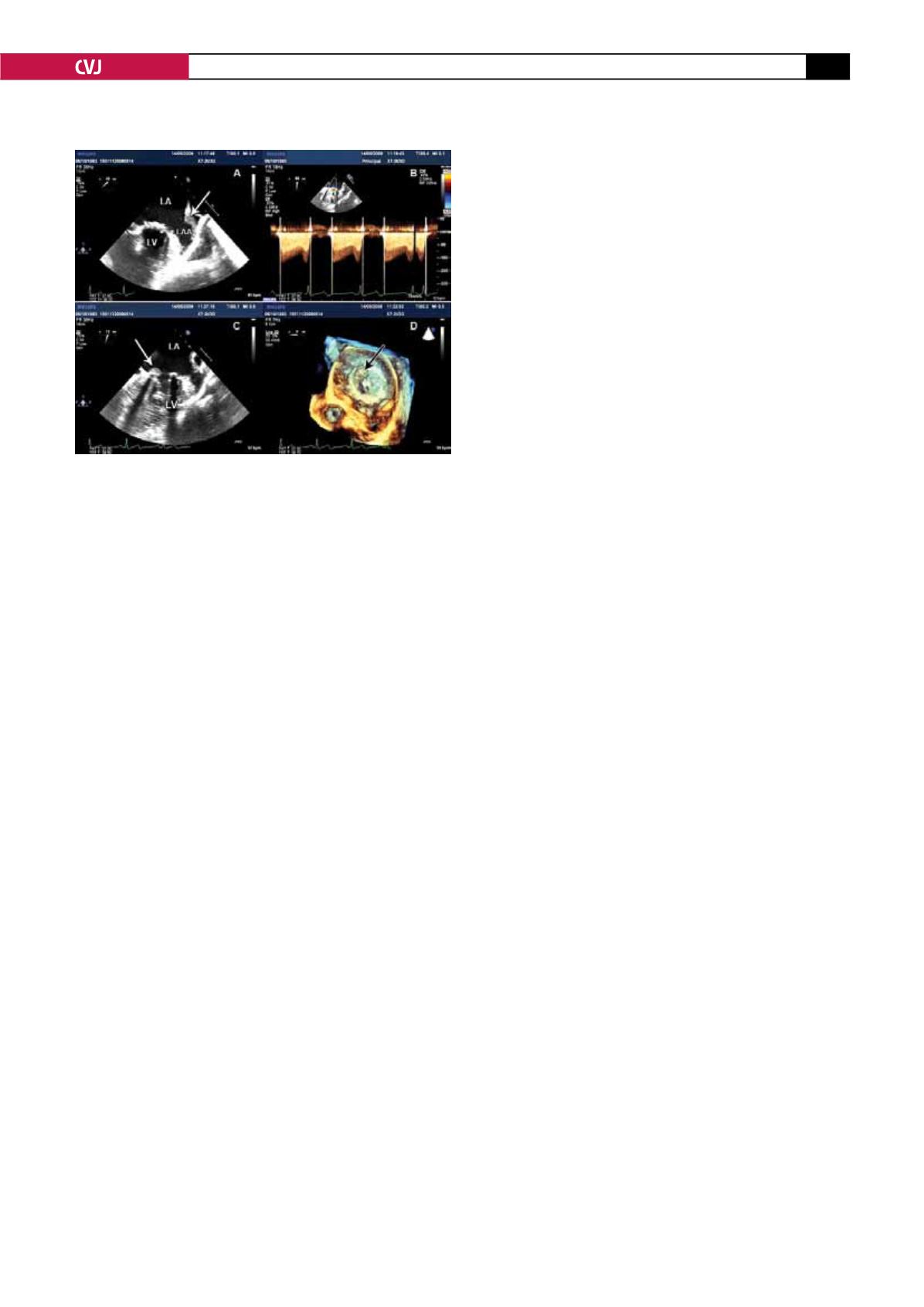
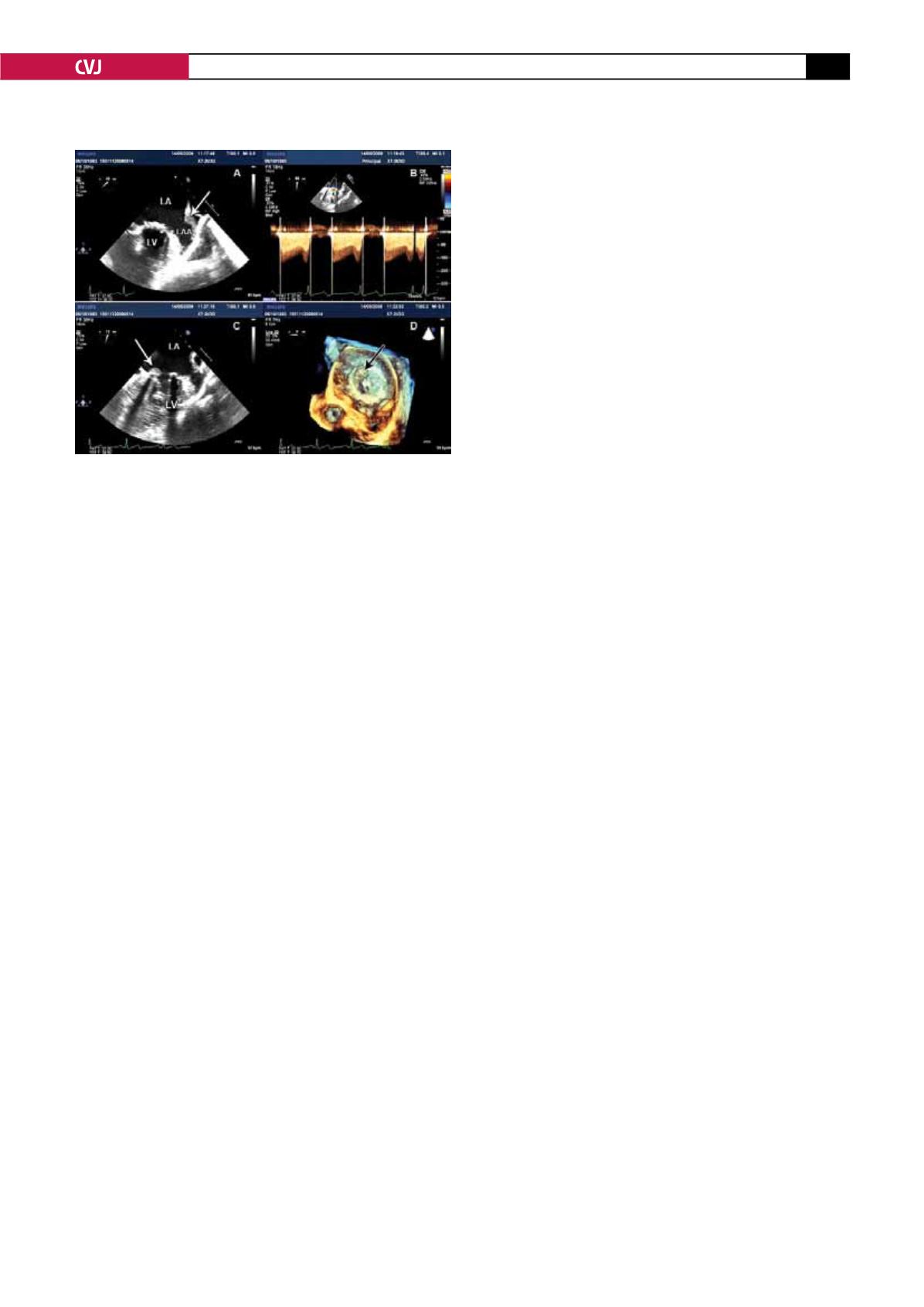
Two-dimensional echocardiography showed an enlarged left
atrium and normal left ventricle with paradoxical septal motion.
Doppler interrogation of the mitral valve prosthesis showed a
maximum gradient of 21 mmHg, a mean gradient of 16 mmHg,
and a mitral valve area of 0.71 cm
2
, consistent with a dysfunc-
tional prosthetic valve.
TEE revealed a thrombus in the left atrial appendage (LAA)
(Fig. 1A), a thrombus in the atrial side of the prosthesis, with
minimal excursion of the disc (Fig 1C). TEE confirmed the
gradients and mitral area found on TTE (Fig. 1B). The real-time
three-dimensional TEE zoom-mode acquisition, frontal view of
the left atrium showed a large thrombus in the valve (Fig. 1D)
and in the LAA.
According to protocol, the patient received recombinant
streptokinase (rSK) 250 000 IU within 30 minutes (charge dose),
followed by 100 000 UI per hour over 72 hours. Unfractionated
heparin was introduced immediately after discontinuation of
rSK, and warfarin and aspirin were administered 24 hours later.
A dramatic improvement in symptoms was observed. The
metallic S1 heart sound became audible and the diastolic rumble
disappeared. There was no evidence of embolic complications
or bleeding. Seventy-two hours after admission, TTE showed a
dramatic improvement in the mitral valve area (1.15 cm
2
) and
the mean gradient fell to 6 mmHg. A chest X-ray five days after
admission showed no pulmonary interstitial oedema.
On discharge, the patient was on therapeutic warfarin, aspirin
100 mg, furosemido 20 mg and bisoprolol 2.5 mg per day, and
was in NYHA class I. The mitral valve area and the mean gradi-
ent were 1.76 cm
2
and 6 mmHg, respectively.
Discussion
PVT is a serious complication of valve replacement, associated
with high mortality rates. The main pathogenic factors of PVT
have been identified, including mitral position of the prosthe-
sis, type of prosthesis, atrial fibrillation, atrial enlargement,
ventricular dysfunction, multivalve replacements, and pregnan-
cy. However, the most common cause is a sub-therapeutic level
of anticoagulation,
1
which had been the case with our patient
(the patient had stopped taking warfarin two months earlier).
This shows the importance of adherence by these patients to
their antithrombotic treatment, and the necessity of INR control.
When PVT is first suspected, a careful physical examination
should be performed, with particular attention being paid to
muffling or disappearance of prosthetic sounds and the appear-
ance of a new regurgitant or obstructive murmur. The initial
diagnostic work up includes transthoracic echocardiography and
cinefluoroscopy for mechanical valves.
2
Transthoracic Doppler
echocardiography is the imaging technique more frequently
used.
PVT may be suspected with increased transvalvular gradients.
However, this measurement is non-specific as the gradient may
be increased by other conditions. On the other hand, normal
gradients do not rule out obstruction in the presence of left
ventricular dysfunction or hypovolaemia.
3
Cinefluoroscopy is an important part of the diagnostic evalu-
ation of a suspected PVT, however this technique is not helpful
in identifying non-obstructive PVT or differentiating pannus
from thrombus.
2,3
Transoesophageal echocardiography is the
diagnostic tool with a higher sensitivity for identifying an abnor-
mal cardiac mass. Moreover, TTE provides important additional
information to guide therapy and is often performed to complete
the investigation.
2
Recent reports show that diagnostic use of three-dimensional
real-time TEE offered a useful and comprehensive evaluation of
prosthetic thromboses (number, size and precise location).
4
In
spite of its unique features, it is not clear if this new technique
is cost effective in the management of PVT. Certainly, more
information is needed.
In our case, we used three echocardiographic modalities (TTE
Doppler, TEE, real-time 3D TEE) to complement each other in
the diagnosis of the PVT and for guidance in the thrombolytic
therapy.
Emergency surgical treatment (thrombectomy or valve
replacement) has been considered the traditional management
for PVT. However, recent surgical series report high mortality,
particularly in severe NHYA functional classes. Durrleman
et
al
.
5
presented a series of 39 patients with PVT over a 20-year
period, who underwent thrombectomy or valve replacement, with
an associated mortality of 25 and 41%, respectively. Oskokeli
et
al
.,
6
in 30 patients with left-side PVT, reported a post-operative
early hospital mortality of 7.1% (NYHA classes II–III) and
31.3% (NYHA class IV), and Toker
et al
.,
7
in 63 cases, a total
mortality of 20.6%.
The current guidelines for the management of PVT remain
controversial. Recent guidelines still recommend surgery as
first-line therapy in critically ill patients (NYHA class III–IV)
Fig. 1. Transoesophageal echocardiography. A: show-
ing thrombus in the left arterial appendage (arrow). B:
confirming the data of TTE (gradients in mitral valve
area). C: showing thrombus in atrial face of the mitral
valve prosthesis (arrow). D: showing the real-time three-
dimensional (frontal view from the atrium) appearance of
the thrombus (arrow) in the mitral valve prosthesis, and
the limited diastolic excursion of the disc. LA: left atrium,
LAA: left arterial appendage, LV: left ventricle.