CARDIOVASCULAR JOURNAL OF AFRICA • Vol 22, No 6, November/December 2011
336
AFRICA
described this syndrome in two patients with sudden onset of
abdominal pain, constipation and large bowel dilatation without
an organic cause of obstruction.
7
The syndrome is therefore
known as Ogilvie’s syndrome. Even though the pathophysiol-
ogy of ACPO is not fully demonstrated, it is deemed to be the
result of large bowel parasympathetic dysfunction.
6
Agents that
increase parasympathetic tone have been shown to be successful
in resolving pseudo-obstruction without colonic decompression
or surgical manipulation. Various studies have shown initial
success rates between 73 and 88% and long-term response rates
between 88 and 100% with the use of neostigmine methyl sulfate
in patients with this condition.
8
Appropriate assessment of the markedly dilated colon involves
urgent gastroenterological evaluation to rule out any cause
of obstruction because this condition may lead to subsequent
ischaemia and perforation of the colon.
8
It is encountered after
almost all types of surgical procedures, including cardiac surgery.
ACPO is characterised by abdominal distension, nausea and/
or vomiting, with failure to pass flatus and stools, and occurs in
up to 60% of patients.
8
In 3 to 15% of patients, massive colonic
dilatation may cause ischaemia and perforation, with subsequent
clinical findings of peritonitis.
6
There is no common size of
caecal distension mandating intervention. According to vari-
ous authors, surgical treatment is indicated if the caecal size is
greater than 8 to 12 cm. However, the symptoms, the patient’s
condition, and progression of the disease are considered when
deciding on surgical intervention.
9,10
ACPO occurs in about 1% of hospitalised patients and
0.046% of patients undergoing CABG surgery.
6
The prevalence
is higher in late middle age (around 60 years) and it is slightly
more common (60%) in men. Because of delayed diagnosis and
inappropriate treatment, ACPO is responsible for considerable
morbidity, with an overall mortality rate of 25 to 31%, and 40 to
50% of patients developing ischaemia or perforation.
8
Diagnosis relies on accurate clinical observation and simple
abdominal radiography, showing variable degrees of colonic
dilatation, mainly involving the proximal colon. A water-soluble
contrast enema (a sensitivity of 96% and specificity of 98%)
or computed tomography (a sensitivity and specificity of 91%)
should be performed to differentiate mechanical obstruction
from pseudo-obstruction.
8
Based on the concept of parasympathetic dysfunction, intrave-
nous neostigmine has been tested in controlled trials and remains
the mainstay of treatment. In various studies, the success rate
of neostigmine treatment has been shown to be 73 to 94% after
the first dose, and up to 100% after the second.
8
Conservative
treatment consisting of a nasogastric tube, fluid resuscitation
and enemas may be helpful in almost half the patients (53%).
Colonoscopic decompression is successful in 77% of patients,
but there is a high rate of recurrence and complications associ-
ated with the procedure.
6
Therefore colonoscopic or surgical
decompression is reserved for situations when conservative
treatment fails, or if the caecum is on the verge of perforation.
In our case, haemodialysis, fluid restriction due to low urine
output, lack of early mobilisation because of surgical complica-
tions and multiple blood transfusions may have contributed to the
occurrence of ACPO. Additionally, calorie, fluid and electrolyte
administration was not optimal in our case because of general-
ised oedema and the patient’s dependence on dialysis. This is an
unfavorable situation in a postoperative patient.
Conclusion
Although ACPO is an unexpected and rare complication after
CABG surgery, rapid and effective treatment is generally
possible with neostigmine. Therefore, early recognition of this
syndrome is important to prevent fatal complications.
References
1.
Alebouyeh N, Toefigh M, Ghasemzadeh N, Mirheydari S, Azargashb E.
Predictors of gastrointestinal perforation in patients undergoing coro-
nary artery bypass graft (CABG) surgery in Tehran, Iran.
Ann Thorac
Cardiovasc Surg
2007;
13
(4): 251–253.
2.
Ghosh S, Roberts N, Firmin R, Jameson J, Spyt TJ. Risk factors for
intestinal ischemia in cardiac surgical patients.
Eur J Cardiothorac Surg
2002;
21
: 411–416.
3.
Yilmaz AT, Arslan M, Demirkilic U, Ozal E, Kuralay E, Bingol H,
et al
. Gastrointestinal complications after cardiac surgery.
Eur J
Cardiothorac Surg
1996;
10
: 763–767.
4.
Recht MH, Smith JM, Woods SE, Engel AM, Hiratzka LF. Predictors
and outcomes of gastrointestinal complications in patients undergoing
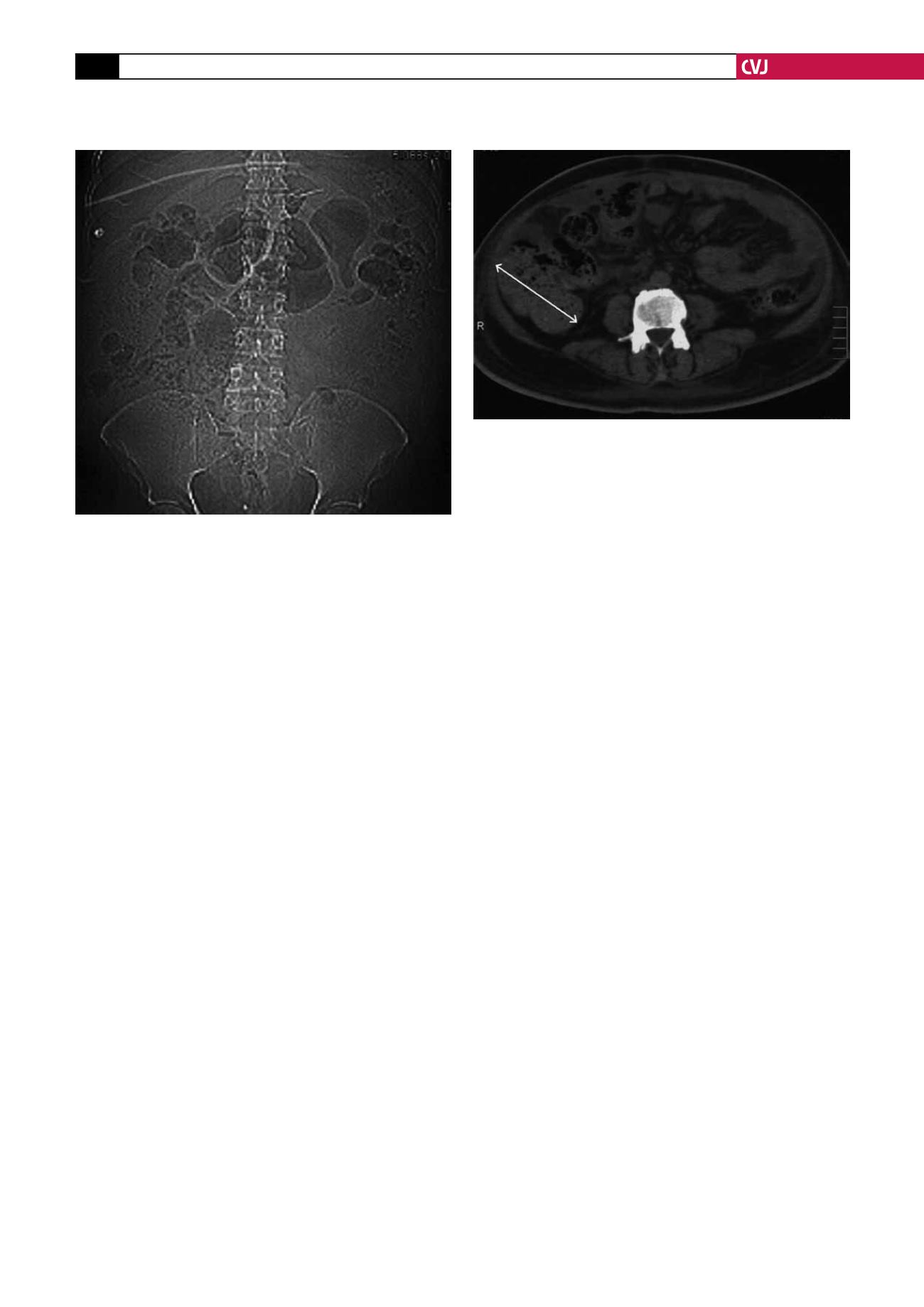
Fig. 2. Caecal dilatation of around 11 cm is shown in
abdominal computerised tomography.
Fig. 1. Abdominal antero-posterior radiography in the
erect position shows high-grade colonic distension.