CARDIOVASCULAR JOURNAL OF AFRICA • Vol 23, No 6, July 2012
316
AFRICA
patients with elevated homocysteine levels compared to those
with normal homocysteine levels. This again suggests that higher
homocysteine levels are seen in patients with established and
more extensive disease, often resulting in a dilated left ventricle
and reduced left ventricular pump efficacy. This correlation
between plasma homocysteine level and poorer left ventricular
function has been noted in other studies.
1
The lack of the statistical significance with multivariate
regression analysis of other indices, except age, suggests that
elevated plasma homocysteine level may well be an independent
risk factor for the presence of CAD, as noted in earlier studies.
25,26
We did however demonstrate a significant relationship between
the number of risk factors for CAD present in a patient and the
presence of elevated plasma homocysteine level.
Most of the patients involved in our study had relatively well-
controlled diabetes, hypertension and dyslipidaemia. Despite
good control in the study group for these risk factors, there
was a higher percentage of patients with increased plasma
homocysteine levels among those patients with higher numbers
of risk factors for CAD (Table 2). This finding is consistent
with several studies
27,28
that show an association of diabetes,
hypertension and smoking with plasma homocysteine levels.
This would suggest that despite the association of plasma
homocysteine level with smoking, diabetes and hypertension,
control of these risk factors does not necessarily result in reduced
homocysteine levels. The treatment of underlying risk factors
may therefore not provide any benefit to the added risk for CAD,
due to the elevated plasma homocysteine levels. These facts may
further explain the failure of homocysteine-lowering therapy to
reduce cardiac events, as these treatments may be given too late
and the raised homocysteine level is less a cause than a marker
of established disease.
However, several mechanisms have been proposed for the
adverse effects of homocysteine on the endothelium of blood
vessels, including coronary arteries. These effects include:
decreased bioavailability of nitric oxide, homocysteine-induced
oxidative stress, and vascular smooth muscle proliferation,
among others.
27-30
Most of these mechanisms also underlie the
mechanism by which other risk factors such as diabetes cause
endothelial dysfunction.
It may also be postulated that homocysteine initiates the
endothelial dysfunction that underlies the CAD, and that once
initiated, it is self-propagating, again explaining the link between
plasma homocysteine level and the degree of established
heart disease, especially as seen with myocardial perfusion
scintigraphy.
29,31
This would confirm that lowering homocysteine
levels at this late stage in the disease process would offer no
benefit.
It has also recently been demonstrated using SPECT
myocardial imaging that disease duration and type of therapy
provide independent and incremental prognostic information for
coronary artery disease in patients with diabetes.
29,31
Patients with
elevated homocysteine levels had significantly lower BMI with
no significant correlation between homocysteine level and BMI.
The lack of significant association was similar to the findings
by some groups,
32
although other groups found at least a weak
correlation.
33,34
The statistical significance (
p
>
0.038) for age in the multi-
variate regression analysis was also noted by previous investi-
gators.
31
This was probably due to the fact that modifiable risk
factors for coronary artery disease, such as diabetes mellitus,
hypertension and dyslipidaemia increase with age. Therefore,
although age was a risk factor, it was not an independent risk
factor for CAD. Finally, the prevalence of elevated homocysteine
levels in our study population was similar to previous work done
on the prevalence in angiographically proven patients with coro-
nary artery disease in Pretoria, South Africa,
35
showing there was
no significant bias in the patient selection for this study.
A limitation to the study was the reliance on semi-automated
analysis of the perfusion indices and LVEF without angiographic
correlation. However the advantage of using such a method is the
reduction in subjective influence by the operator.
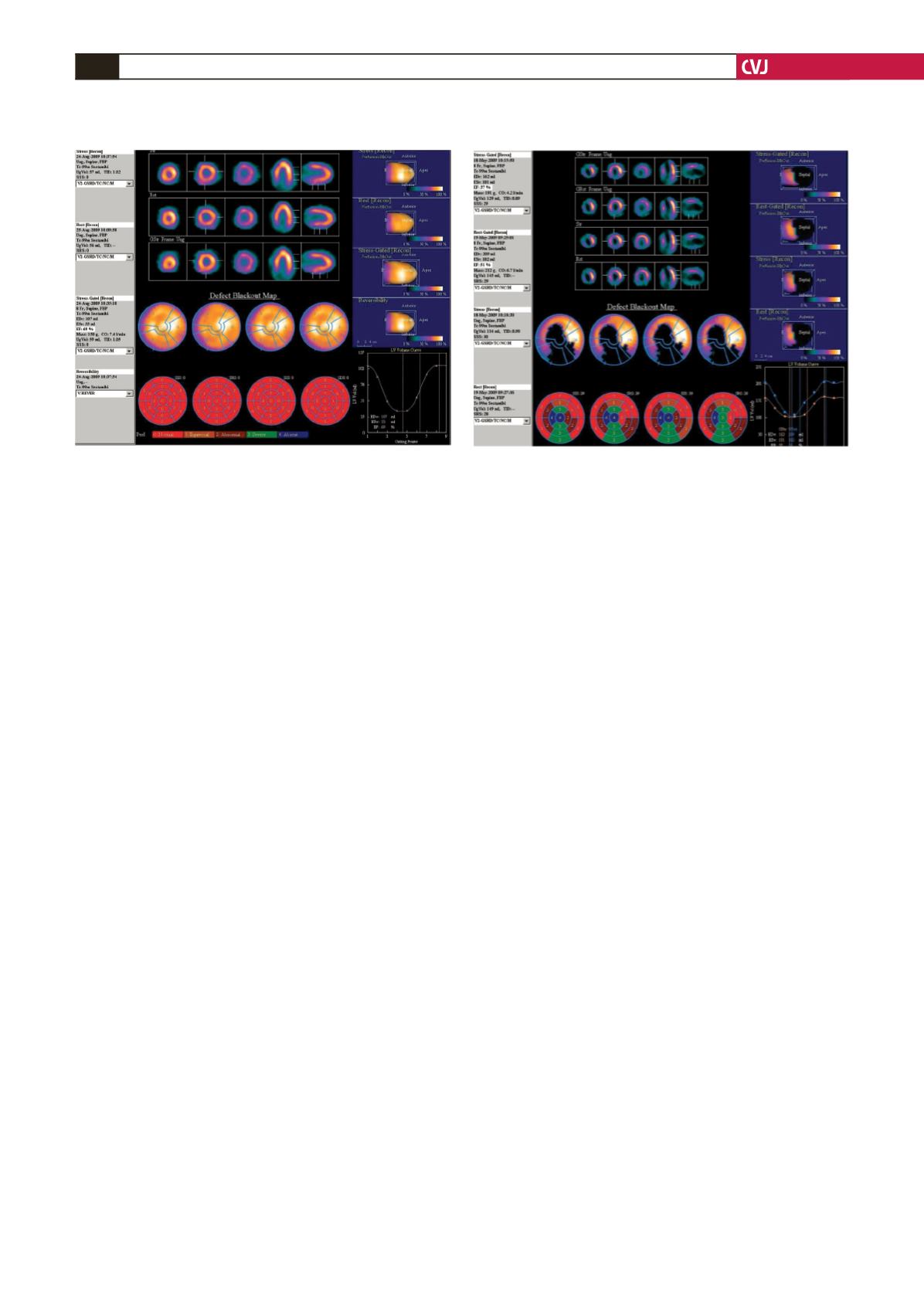
Fig. 1. Myocardial perfusion scintigraphy and ‘bullseye’
plots of a 48-year-old male with diabetes, hypertension,
dyslipidaemia and significant smoking history. His plas-
ma homocysteine level was normal (7
μ
mol/l). There was
normal perfusion at stress and rest, and the left ventricu-
lar ejection fraction was normal (69%).
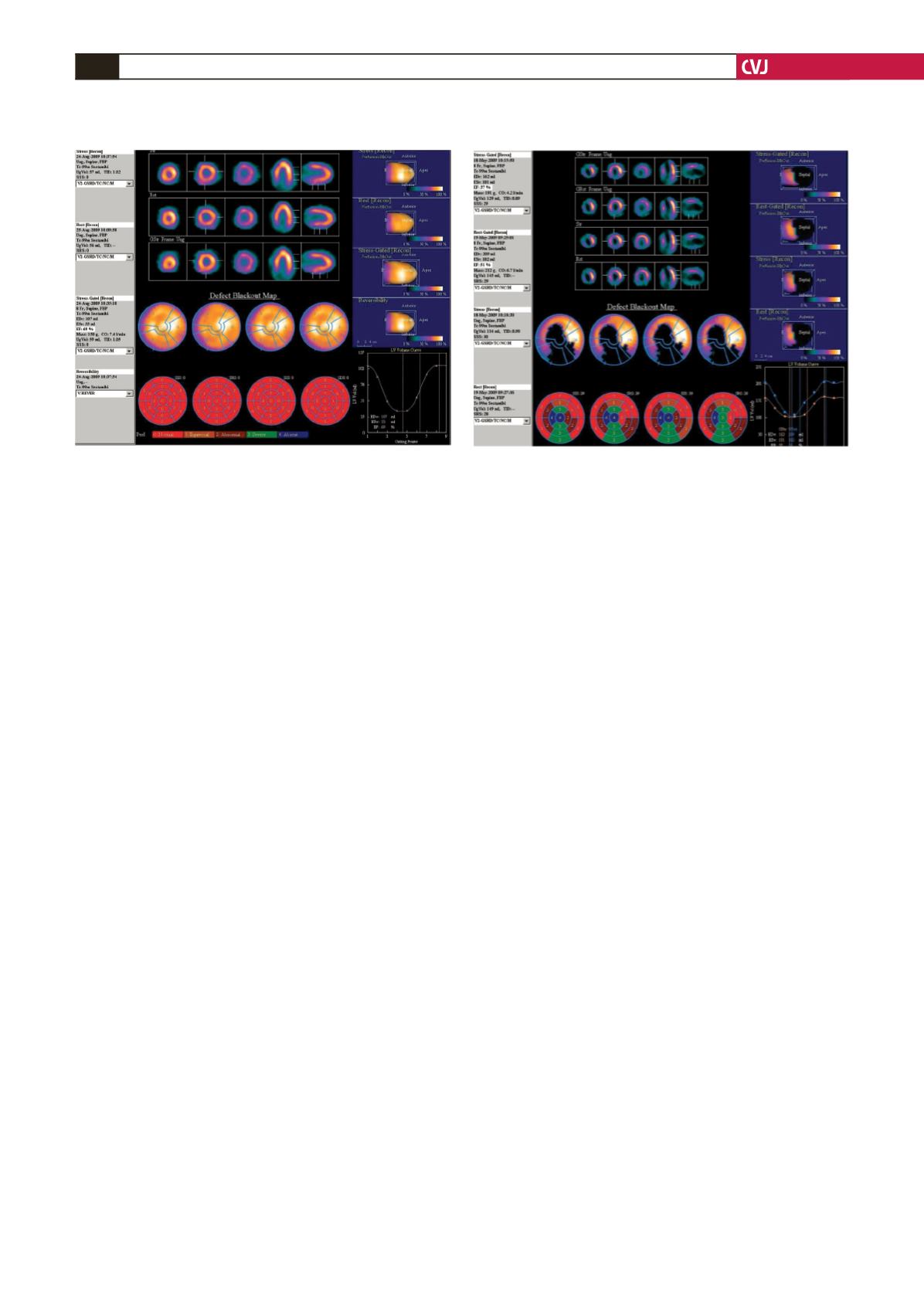
Fig. 2. Myocardial perfusion scintigraphy and ‘bullseye’
plots of a 49-year-old male with diabetes, hypertension
and significant smoking history. His plasma homocys-
teine level was elevated (13
μ
mol/l).
99m
Tc MIBI imaging at
stress and rest showed a significant persistent defect in
the anterior wall, apex and inferior wall, with no concur-
rent ischaemia. The left ventricular ejection fraction was
reduced (37%).