CARDIOVASCULAR JOURNAL OF AFRICA • Vol 23, No 7, August 2012
368
AFRICA
Streptokinase was the thrombolytic agent of choice in 54.5%,
TNK-tPA in 30.3%, t-PA in 10.1% and r-PA in 5.1% of patients.
The thrombolytic therapy was administered in association with
LMWH in 36% and UFH in 26% of subjects. In 11% of patients,
glycoprotein IIb/IIIa inhibitors were given on the same day as
the thrombolytic therapy. This may reflect usage due to failed
reperfusion and patients being referred for urgent rescue PCI.
Overall, 93% of patients underwent angiography (90.1% of
STEMI and 95.0% of NSTE-ACS patients). Fifty-three per cent
went on to have PCI (59.7% of STEMI and 49.4% of NSTE-
ACS patients), while 14.6% were referred for CABG (7.9%
of STEMI and 19.3% of NSTE-ACS subjects). Of the patients
referred for PCI, 94.2% had at least one stent inserted (92.1%
of STEMI and 96.1% of NSTE-ACS patients), and in 57.9% of
cases (51.8% of STEMI and 62.8% of NSTE-ACS patients), this
was a drug-eluting stent. PCI was performed within 24 hours
of hospitalisation in 61.3% of cases. There were 88 patients
(34.8%) who received thrombolytic therapy but who did not
exhibit reperfusion and were taken for PCI on the first day of
hospitalisation.
Most patients (94% of STEMI and NSTE-ACS subjects)
received aspirin, 29.3% received a glycoprotein IIb/IIIa inhibitor,
58.7% a thienopyridine loading dose, and 65.9% a thienopyridine
maintenance dose. All thienopyridine use was clopidogrel.
UFH heparin was used in 39.7% of patients, and LMWH in
63.4%. The LMWH was almost exclusively enoxaparin. During
hospitalisation, 560 (91.1%) patients received a statin, 13.2%
a calcium channel blocker (CCB), 69.9% a beta-blocker (BB),
61.1% an angiotensin converting enzyme inhibitor (ACEI) and
5.2% an angiotensin II receptor blocker (ARB). In-hospital
bleeding was reported in 21 patients (3.4%); 12 (4.7%) with
STEMI and nine (2.5%) with NSTE-ACS.
Post-hospital management and follow up
Ninety-two per cent of patients were discharged from hospital
on aspirin, 62.2% on clopidogrel, 93.3% on a statin, 13.6% on a
CCB, 67.4% on a beta-blocker, 61.4% on an ACE inhibitor, and
5.9% on an ARB (Table 3). The rates of use of these drugs were
higher among patients with STEMI than in those with NSTE-
ACS, with the exception of the use of ARBs.
Follow-up information was obtained telephonically in 58%
of cases. At 12 months, 91 (15.6%) patients had had at least
one further cardiac-related hospitalisation (41 for STEMI and
50 for NSTE-ACS patients). Unstable angina (i.e. no cardiac
biomarker elevation) was the reason for re-hospitalisation in
49 (8.6%) cases and occurred 166 days (mean) after the index
hospitalisation. Only four patients were re-admitted for NSTE-
ACS and six for STEMI, 253 and 116 days (mean) after the
index hospitalisation, respectively. Six patients reported stroke
or TIA following hospitalisation and there were 14 re-admissions
for heart failure. Bleeding episodes after discharge from hospital
for the primary event occurred in 10 (1.8%) of the subjects, five
(2.2%) in STEMI and five (1.5%) in NSTE-ACS patients.
At one year, 80.2% of patients were still taking aspirin, 77.3%
statin,19% clopidogrel, 10.3% CCB, 53.8% beta-blockers, 46%
ACE inhibitors, and 3.8% ARB.
Thirty-day death rates were 2.4% for STEMI and 1.7%
for NSTE-ACS patients. Thirty-five patients (5.7%) had died
by one year (
±
35 days). The one-year mortality rate for
patients admitted for STEMI was 6.7% and for NSTE-ACS,
5.0%. Causes of death were fatal MI (eight patients), fatal
stroke (two), other cardiovascular including sudden death (12),
non-cardiovascular (six), and unknown (seven). Predictors of the
primary endpoint outcome (all-cause death at one year) were age
≥
70 years (
p
=
0.0049), history of stroke/TIA (
p
=
0.0396), and
diabetes (
p
=
0.0439).
Discussion
This registry is the first in South Africa to document the
demographics and management strategies used in patients
admitted to hospital with a diagnosis of acute coronary syndrome.
Patients with pre-existing risk factors of hypertension, diabetes
and/or dyslipidaemia were more likely to present with NSTE-
ACS, while smokers were more likely to present with STEMI.
STEMI patients were also younger than NSTE-ACS patients.
Although age
≥
70 years was a predictor of one-year mortality,
the mortality rates in the two groups were similar.
Thrombolysis was performed in a minority of patients despite
a lack of contraindications. This may reflect the availability of
urgent angiography at most of the enrolling centres. Almost all
patients were referred for angiography with high intervention
rates. There was a preference for the use of drug-eluting stents
as opposed to bare metal stents. Revascularisation rates were
high and certainly higher than the overall ACCESS data (68.5
vs 40.8%), but were similar for NSTE-ACS and STEMI (68.75
and 68.6%) patients. Therefore, approximately one-third of all
patients were being treated conservatively/medically only.
The use of appropriate ancillary drug therapy in hospital and
on discharge was in line with other registries; more than 90%
receiving a statin, 70% a beta-blocker and 70% some form of
RAAS blockade. As to be expected, the use of calcium channel
blockers was low (13%).
Use of anti-thrombotic therapy was also in keeping with
guidelines; 94% receiving aspirin, two-thirds clopidogrel, and
65% heparin (with LMWH being used more commonly).
However, the use of a thienopyridine at discharge was lower in
the South African cohort (62.2%) compared with the ACCESS
population (76.1%), despite a higher intervention rate and
usage of stents, and in particular, drug-eluting stents. One has
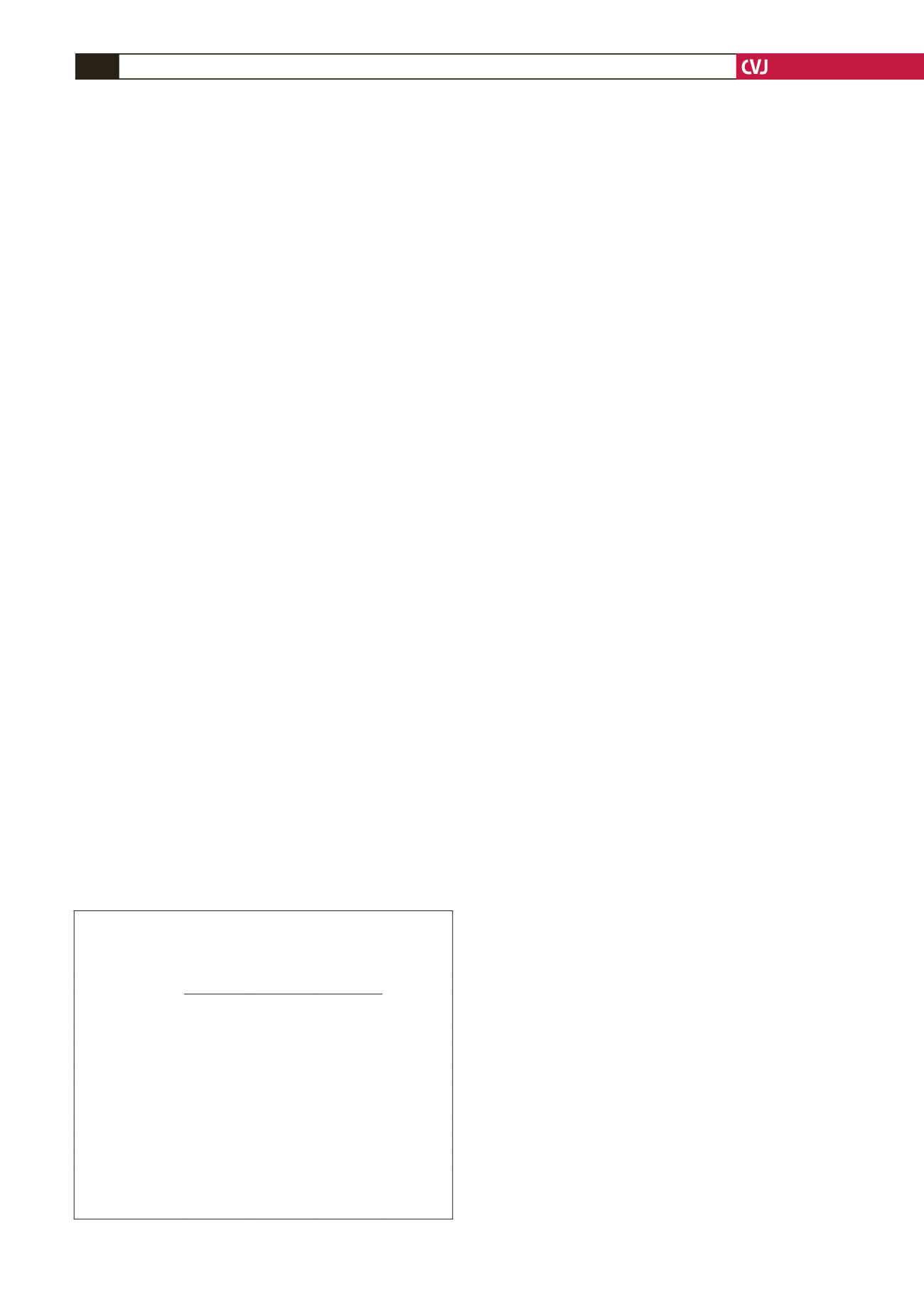
TABLE 3. SELECTED DRUGTREATMENTSAT DISCHARGE:
SOUTHAFRICAN COHORTACCORDINGTO
DISCHARGE DIAGNOSISAND OVERALL,
AND COMPLETEACCESS STUDY OVERALL
Discharge drug
treatments
South Africa
ACCESS
NSTE-ACS
(
n
=
360)
STEMI
(
n
=
251)
All
(
n
=
611)
All
(
n
=
11 427)
Aspirin
333 (92.5) 233 (92.8) 566 (92.6)
90.1
Thienopyridine
208 (57.8) 172 (68.5) 380 (62.2)
76.1
Statin
330 (91.7) 240 (95.6) 570 (93.3)
89.2
Calcium channel
blockers
65 (18.1)
18 (7.2)
83 (13.6)
16.5
Beta-blocker
222 (61.7) 190 (75.7) 412 (67.4)
75.8
ACE inhibitor
195 (54.2) 180 (71.7) 375 (61.4)
64.3
ARB
26 (7.2)
10 (4)
36 (5.9)
11.3
ARB: angiotensin receptor blocker
Unless otherwise indicated result are reported as number (percent);
ACCESS includes South Africa.