CARDIOVASCULAR JOURNAL OF AFRICA • Vol 24, No 6, July 2013
AFRICA
205
makes it cumbersome and it requires a large delivery system
(5–7 F) (St Jude Medical, Cardiovascular Division, St Paul,
MN). This large delivery system makes it difficult and rather
challenging to close a moderate to large PDA in small infants (
<
6 kg). The device may also cause coarctation of the aorta due to
its large retention skirt, which is on the aortic side.
19
While the ADO II has a low profile and low delivery
system, it can also cause aortic and left pulmonary artery (LPA)
obstruction like the ADO I.
20-22
In this series, there was one
patient who had mild LPA obstruction. Both devices have the
potential to embolise.
21
We had one device that embolised. The patient (patient 15)
had a large PDA with its narrowest diameter being 5.5 mm,
which is the upper limit for percutaneous closure using ADO
II, according to the manufacture’s guidelines (see Table 1). This
patient had a large left-to-right shunt with a Qp:Qs ratio of 2.8:1.
The duct morphology itself was more tubular than conical. The
ductal size and the shape of the PDA were high risk factors
for embolisation in this patient. The device was successfully
retrieved and the duct was deemed unsuitable for percutaneous
closure and as a result was closed surgically.
Care should be taken when choosing a device for closure of
large PDAs with less suitable anatomy, as in such patients, the
device might embolise. There were no major catheterisation-
related complications in this study, such as bleeding, requiring
blood transfusion, loss of femoral arterial pulse or arterial
avulsion, as reported elsewhere.
21,22
The low-profile TorqVue delivery system of the ADO II (4–5
F) allows this device to be used to close PDAs in smaller infants
(
<
6 kg) with a limited risk of causing either aortic or pulmonary
obstruction in carefully selected patients. In this series, there
were 10 patients weighing less than 6 kg who underwent
ductal closure using the ADO II, contrary to the manufacturer’s
recommendations. This device was also able to close ducts in
patients less than six months of age. Eight patients in this study
were younger than six months of age (range 2–5 months).
Another advantage of this device over the ADO I is that
it may be introduced both in anterograde fashion through the
pulmonary side and in retrograde approach through the arterial
side to close the PDA. In this report, there were six patients who
had their ducts closed through the arterial side. Except for one
patient whose duct was 6.2 mm, PDAs less than 3 mm (range
0.6–2 mm) were closed through the aortic route.
Historically, smaller PDAs (
≤
3 mm) would be closed with
Cook’s or Gianturco coils or the Nit Occlud device.
21
The ADO
II has offered an alternative to this mode of closure. It should be
mentioned though that the ADO II remains more expensive than
the Gianturco coils. It has also been shown that the coils have
less screening time and have shown less use of contrast than the
Amplatzer device.
21
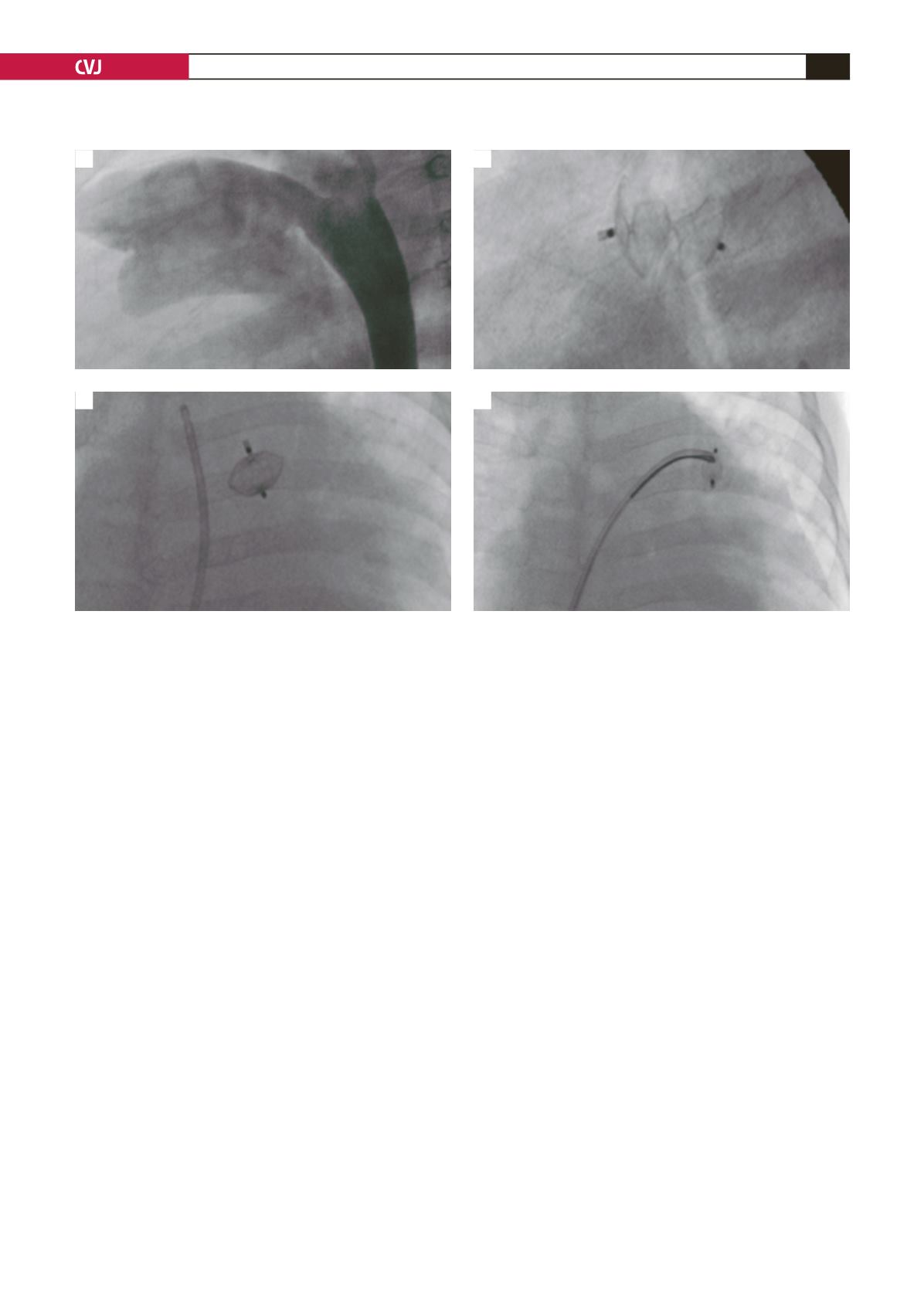
When it comes to ductal shape, other devices such as the ADO
I, coils and Nit Occlud device would close Krichenko type A
(conical) PDAs. The ADO II has been shown in this report (Fig.
4) and others to be able to close all anatomical types of PDAs,
including tubular and long (type C), and tubular, AP-window like
ducts with a shallow aortic ampulla (type B).
17,20,21
Two patients
had residual ducts at three months of follow up. Residual ducts
have been reported in other studies.
23,24
These were closed using
coils or the Nit Occlud device.
In terms of the narrowest diameter of the PDA, the
manufacturer recommends closure of the PDA using the ADO
II up to 5.5 mm. In this series, there was one patient who had a
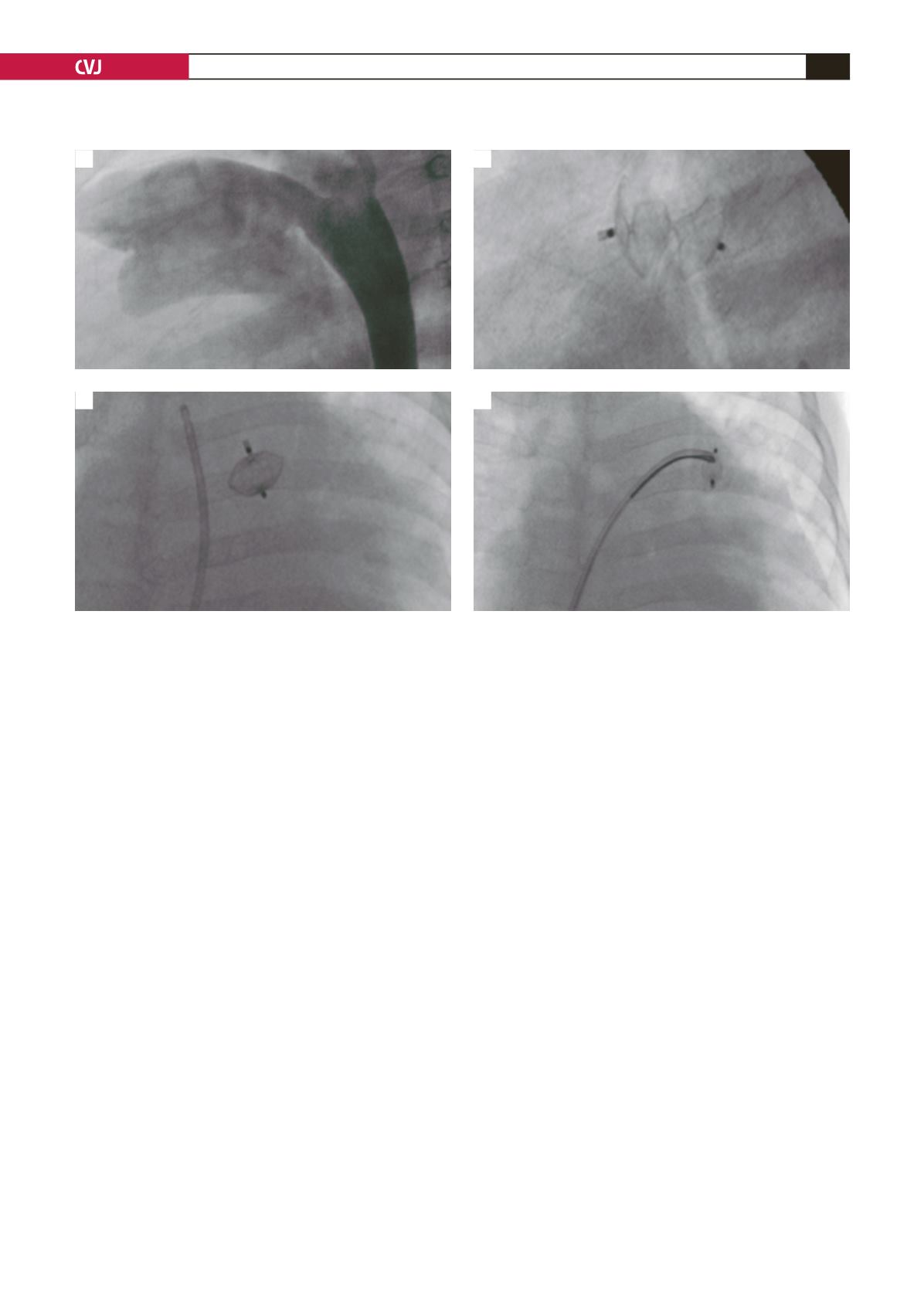
Fig. 3. Large patent ductus arteriosus (PDA) before closure (A); with device in the PDA (B); dislodged device in the
left pulmonary artery (C); and percutaneous retrieval of device (D).
A
C
B
D