CARDIOVASCULAR JOURNAL OF AFRICA • Volume 26, No 1, January/February 2015
10
AFRICA
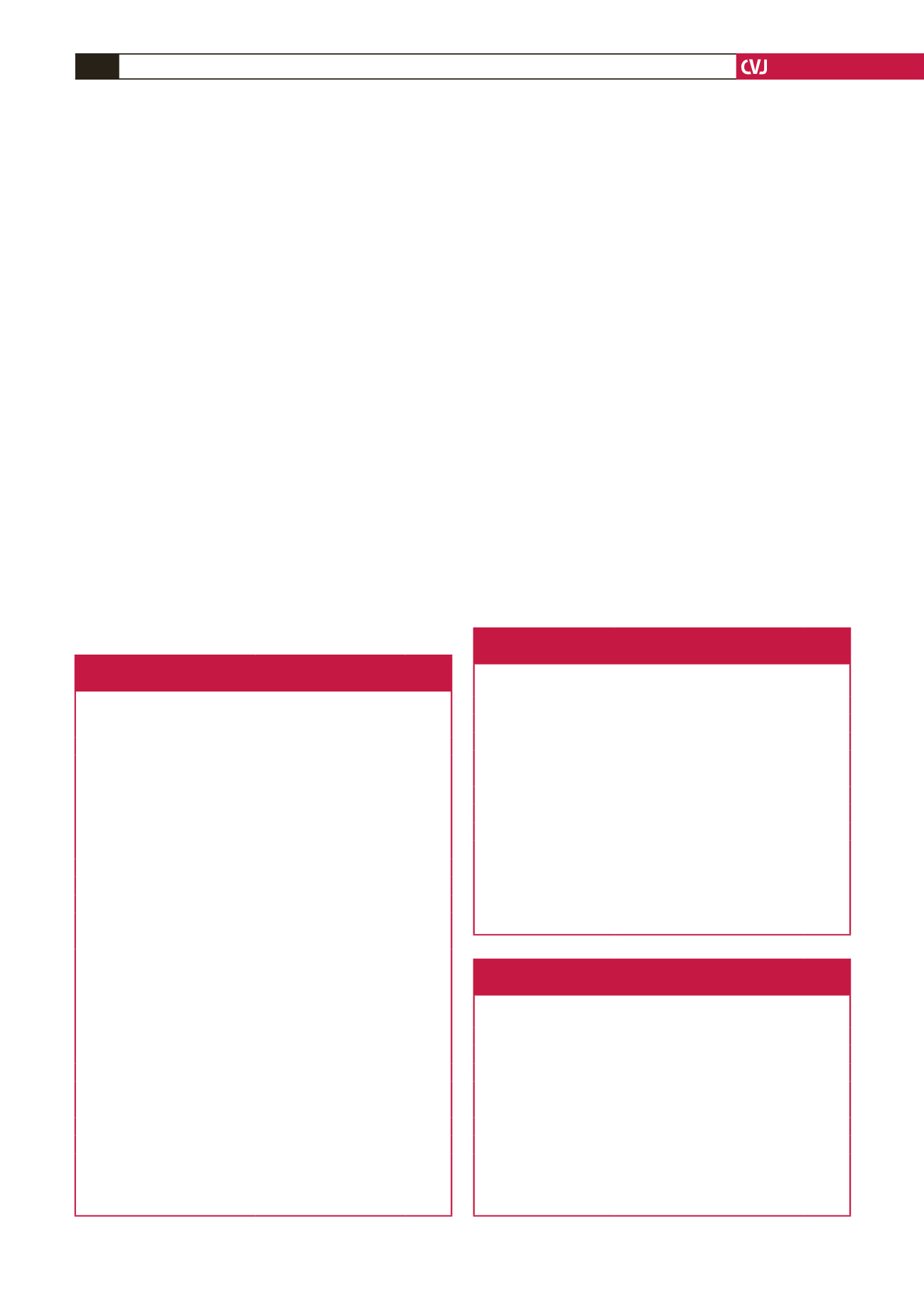
(Table 1). No differences were evident between the groups in terms
of systolic/diastolic blood pressure, heart rate, blood cholesterol
levels and respiratory function test parameters (Table 1).
Asthma patients and the control group were evaluated
with transthoracic echocardiography. There was no significant
difference between the two groups in the measurements of
LVPWTed, LVED, LVES, IVSed, LA, aortic anulus diameter,
EF and FS (Table 2). Mean pulmonary pressure (mPAP) of
the asthma patients was higher than in the control group (19.9
±
7.1 vs 12.6
±
6.2 mmHg) and this difference was statistically
significant (
p
<
0.05). There was no correlation between mPAP
and aortic stiffness parameters (Pearson’s correlation analysis).
In 15 of the asthma patients, echocardiography revealed mild
tricuspid regurgitation and right ventricular systolic pressure
was calculated from regurgitant flow. Average right ventricular
systolic pressure of these 15 patients was 27.2
±
5.7 mmHg. Since
we had evaluated only asthma patients without exacerbation
of their asthma within the previous four weeks, there was
no difference in baseline respiratory function test parameters
between the study and control groups.
There was no significant difference between the asthma and
control groups in the measurements of Ds, Dd, DIS, S, Ep and
Ep* (Table 3). There was no significant correlation between
aortic stiffness parameters and serum total cholesterol (
r
=
0.03), LDL cholesterol (
r
=
0.09), HDL cholesterol (
r
=
0.09)
and triglyceride (
r
=
0.134) levels (Pearson correlation analysis).
There was no correlation between hs-CRP and aortic stiffness
parameters, DIS (
r
=
0.268), Ep (
r
=
0.199), EP* (
r
=
0.150) and
S (
r
=
–0.230).
Out of 50 asthma patients, 18 had intermediate severity
asthma. Aortic stiffness parameters were compared between
these patients and the control group. There was no statistically
significant difference between the two groups (
p
>
0.05) (Table 4).
Twenty-six of the asthma patients were intermittently using
inhalers with short-acting beta-agonists; 10 were also using
montelukast Na together with short-acting beta-agonists.
Twenty-four of the patients were using long-acting inhalers
with beta-agonists together with inhalers with corticosteroids;
16 of them were also using montelukast Na. Since these
asthma drugs have multiple effects on the aortic and peripheral
vascular system, we compared the aortic stiffness parameters of
these different treatment groups. We did not detect statistically
significant differences between the groups (
p
>
0.05).
We evaluated the effects of the presence of atopy and severity
of asthma on aortic stiffness parameters. There was no difference
in aortic stiffness parameters between atopic asthma patients and
the control group (Table 5).
Discussion
The present cross-sectional study was undertaken to
comparatively evaluate the elastic properties of the abdominal
Table 1. Characteristics of the asthma
patients and control group
Asthma
patients
(
n
=
50)
Control
group
(
n
=
57)
p
-value
Gender, female/male
24/26
34/23
>
0.05
Age, years
11.7
±
2.7 12.3
±
2.8
>
0.05
Presence of atopy, %
37 (74)
0 (0)
Immunotherapy
27 (54)
0 (0)
Duration of diagnosis of
asthma, years
8.1
±
2.8
(3–15)
Weight, kg
43.0
±
15.5 47.8
±
17.0
>
0.05
Height, cm
148.0
±
15.9 150.4
±
16.1
>
0.05
BMI, kg/m²
19.0
±
4.1 20.5
±
4.3
>
0.05
Systolic blood pressure, mmHg 101.1
±
10.4 102.4
±
10.4
>
0.05
Diastolic blood pressure, mmHg 63.5
±
9.9 64.9
±
9.8
>
0.05
Mean blood pressure, mmHg
76.0
±
9.2 77.4
±
9.3
>
0.05
Heart rate, beat/min
84
±
15
85
±
14
>
0.05
Total cholesterol, mg/dl (mmol/l) 152.5
±
32.6
(3.96
±
0.84)
147.5
±
24.6
(3.82
±
0.64)
>
0.05
LDL cholesterol, mg/dl (mmol/l) 83.6
±
17.8
(2.17
±
0.46)
79.6
±
18.1
(2.06
±
0.47)
>
0.05
HDL cholesterol, mg/dl
(mmol/l)
55.6
±
17.3
(1.44
±
0.45)
50.7
±
11.5
(1.31
±
0.30)
>
0.05
hs-CRP, mg/dl
2.12
±
0.41 0.79
±
0.20
<
0.05
FVC, % predicted
87.3
±
13.6 87.1
±
10.6
>
0.05
FEV1, % predicted
97.7
±
14.9 99.2
±
11.1
>
0.05
FEV1/FVC, %
95.2
±
5.8 97.0
±
4.3
>
0.05
PEF, % predicted
92.8
±
16.6 89.8
±
14.6
>
0.05
Data are presented as mean
±
standard deviation.
BMI: body mass index, FEV1: forced expiratory volume in one
second, FVC: forced vital capacity, HDL: high-density lipoprotein,
LDL: low-density lipoprotein, PEF: peak expiratory flow.
Table 2. Echocardiographic findings of the
asthma and control groups
Asthma patients
(
n
=
50)
Control group
(
n
=
57)
p
-value
LVPWTed, mm
7.1
±
0.1
7.0
±
0.1
>
0.05
LVED, mm
40.1
±
4.6
40.4
±
4.8
>
0.05
LVES, mm
25.8
±
4.5
24.7
±
3.9
>
0.05
IVSed, mm
7.4
±
1.1
7.2
±
1.1
>
0.05
LA, mm
25.3
±
4.0
23.2
±
3.7
>
0.05
Aortic anulus, mm
16.8
±
3.2
17.1
±
2.6
>
0.05
EF, %
72
±
10
76
±
8
>
0.05
FS, %
36
±
7
38
±
7
>
0.05
mPAP, mmHg
19.9
±
7.1
12.6
±
6.2
<
0.05
Data are presented as mean
±
standard deviation.
EF: ejection fraction, FS: fractional shortening, LA: left atrial
diameter, LVED: left ventricular end-diastolic diameter, LVES: left
ventricular systolic diameter, LVPWTed: end-diastolic left ventricular
posterior wall thickness, mPAP: mean pulmonary artery pressure.
Table 3. Aortic stiffness parameters in the
asthma and control groups
Asthma Patients
(
n
=
50)
Control Group
(
n
=
57)
p
-value
Peak aortic velocity, cm/s 125.6
±
16.7
123.5
±
17.9
>
0.05
Ds, mm
11.4
±
2.0
11.1
±
1.9
>
0.05
Dd, mm
8.2
±
1.5
8.2
±
1.8
>
0.05
DIS, 10
-6
cm
2
/dyne
1.35
±
0.52
1.41
±
0.66
>
0.05
S
0.38
±
0.11
0.37
±
0.14
>
0.05
Ep, N/m
2
107.5
±
39.0
116.5
±
55.9
>
0.05
Ep*
1.75
±
0.73
1.83
±
0.90
>
0.05
Data are presented as mean
±
standard deviation.
Dd: abdominal aorta diastolic diameter, DIS: aortic distensibility, Ds:
abdominal aorta systolic diameter, Ep: pressure strain elastic modulus,
Ep*: pressure strain normalised by diastolic pressure, S: aortic strain.



















