CARDIOVASCULAR JOURNAL OF AFRICA • Vol 23, No 8, September 2012
AFRICA
429
not impair homeostasis.
7
Correcting hypovolaemia with HES has been suggested to
be associated with an increased risk of acute renal failure, and
interest has recently been focused on the influence of HES
solutions on renal function.
8
Boldt
et al.
found better kidney
function and less inflammation with the use of HES than with
albumin solutions.
4
The aim of this study was to compare the effect of 6% hydroxyl
ethyl starch solution with 4% gelatin and Ringer’s solutions on
haemodynamic stability of patients after CABG surgery and
immediately after discontinuation of cardiopulmonary bypass.
Methods
This was a prospective, randomised, double-blind clinical trial
in 92 patients who were candidates for on-pump CABG. The
age range of patients was from 40 to 75 years. Exclusion criteria
were left ventricular ejection fraction
<
40%,
right heart failure,
emergency patients, pump time
>
180
minutes and clamp time
>
90
minutes, patients who needed re-operation within the first six
hours due to surgical haemorrhage or other reasons, renal failure
needing haemodialysis, and those with respiratory failure.
All patients received pre-anesthesia medication. Lorazepam
(1
mg orally) was given the night before the operation and
intramuscular morphine (0.1 mg/kg) one hour before induction
of anaesthesia in all patients. In the operating room, lidocaine
(1%)
was used for access to arterial and peripheral vessels and
Ringer’s crystal solution was administered in a dose of 5–10
ml/kg. Anaesthesia induction was started with intravenous
medazolam sufentanyl and pancranium.
After the use of 100% oxygen by mask, patients were intubated
with an endotracheal tube and connected to a mechanical
ventilator and central venous pressure (CVP) was introduced
in the right internal jugular vein. Maintenance of anaesthesia
was achieved with continuous infusion of idazolam, atrocurium
and sufentanyl. After infusion of 300 IU/ kg heparin, the patient
went on-pump and the activated clotting time (ACT) was above
480
s, mean arterial pressure 60–70 mmHg, haematocrit level
was 22–27%, and the temperature was set at 32°C.
After discontinuation of cardiopulmonary bypass (CPB)
all patients were transferred to the intensive care unit (ICU)
and were randomly divided into three groups. The first group
received Ringer’s solution, the second gelatin (4%), and the
third group hydroxyl ethyl starch solution (HES) (6%) (Voluven)
as a volume expander to maintain the CVP between 7 and 14
mmHg. Packed cells were infused where the haemoglobin level
was lower than 8 mg/dl and fresh frozen plasma (FFP) was used
for continuous bleeding with a normal range of ACT and APTT
(
activated partial thromboplastin time).
Cardiac output was monitored with a NICO instrument
and haemodynamic values were monitored continuously. In
situations where, after maintaining adequate volume, the mean
arterial pressure was below 60 mmHg and cardiac index below
2
l/min/m
2
body surface area, inotrope infusion (dobutamine or
epinephrine) was started.
Haemodynamic parameters such as heart rate, mean arterial
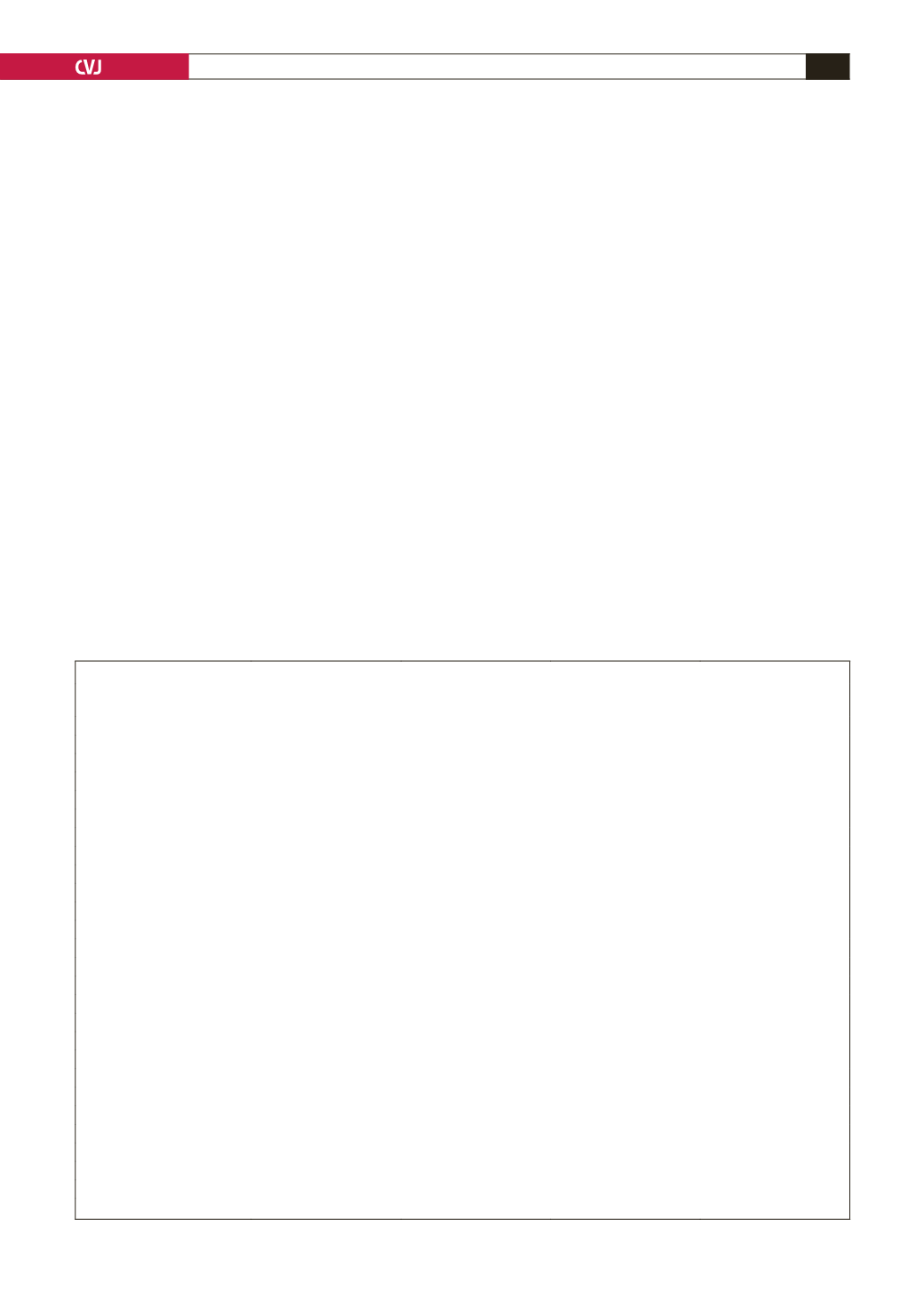
TABLE 1. DEMOGRAPHIC CHARACTERISTICS OF PATIENTS (
±
SD)
Ringer’s solution
(
n
=
29)
Gelatin (4%)
(
n
=
31)
HES (6%)
(
n
=
32)
p
-
value
Age (year)
59 (11)
60 (8.7)
57 (10.4)
0.495
Weight (kg)
73.4 (10.8)
72.5 (11.9)
74.4 (11)
0.795
Height (cm)
167.4 (8.2)
165 (8.3)
167 (6.7)
0.750
Ejection fraction %
41 (8.4)
45 (6.7)
46 (5.9)
0.195
Numbers of bypass
3 (0.3)
3 (0.4)
2.9 (0.4)
0.449
Drug usage:
Plavix
1
4
0
0.283
Beta-blocker
26
22
21
0.78
ASA
17
19
18
0.410
ACE inhibitors
15
16
17
0.380
Nitrates
14
12
13
0.210
Oral antidiabetic agents
7
8
7
0.150
Other antihypertensive agents
5
6
5
0.110
Diuretics
13
11
12
0.225
Anesthesia time (min)
263 (191–310)
250 (181–301)
247 (185–305)
0.140
CPB time (min)
109 (37)
99 (28)
106 (34)
0.120
Cross-clamp time (min)
63 (26)
55 (20)
59 (25)
0.170
Systolic BP (mmHg)
120 (11)
123 (16)
114 (9)
0.211
Diastolic BP (mmHg)
75 (11)
73 (10)
70 (9)
0.293
Na (meq)
134 (7)
140 (9)
135 (20)
0.212
K (meq)
4.3 (0.44)
4.3 (0.47)
4.35 (0.45)
0.143
PTT (s)
30 (4.5)
35 (5.3)
29 (5)
0.136
INR
1.1 (0.25)
1.08 (0.2)
1.08 (0.16)
0.278
Haemoglobin (g/dl)
12.7 (8.1–15)
12 (9–14)
12.3 (8.4–13.5)
0.323
BUN (g/dl)
13 (9–23)
15 (9–31)
15.5 (9–23)
0.275
Creatinine (g/dl)
0.9 (0.7–1.04)
0.95 (0.5–1.3)
1(0.7–1)
0.340
CBP: cardiopulmonary bypass, BP: blood pressure, ACE: angiotensin converting enzyme, PTT: partial thromboplastin time.