CARDIOVASCULAR JOURNAL OF AFRICA • Vol 24, No 9/10, October/November 2013
e14
AFRICA
ng/l; creatine kinase MB, 210 mmol/l; myoglobin, 124 mmol/l;
BNP 1 046 ng/ml; and no abnormalities in renal function,
electrolyte parameters or routine blood and urine tests. A
diagnosis of acute anterior myocardial infarction was established.
The patient and her family declined an emergency coronary
angiography test and treatment. She was given oxygen, ECG
monitoring, oral enteric-coated aspirin tablets (300 mg),
clopidogrel (300 mg), rosuvastatin calcium (10 mg) and a
subcutaneous injection of low-molecular weight heparin calcium
(5 000 U). Intravenous thrombolytic therapy with urokinase
(200 U) was immediately performed. However, there were
no significant changes in the ECG after 30 minutes or one
hour, and after 1.5 hours, the patient became irritable, her face
became pale grey, and she began sweating. The patient’s blood
pressure dropped to 70/30 mmHg, and she presented with sinus
bradycardia, third-degree atrio-ventricular block, a ventricular
rate of 33 beats/min and unconsciousness. Atropine was applied
through intravenous injection, which was immediately followed
by ventricular tachycardia and ventricular fibrillation. After three
defibrillation attempts (200 J), sinus rhythm was restored, and
the heart rate was 130–160 beats/min.
After one hour, the patient regained consciousness and reported
chest tightness and shortness of breath, and exhibited a pale grey
face and cold limbs. Dopamine (3 120 mg), norepinephrine
(2 mg), metaraminol (160 mg) and dobutamine (1 640 mg)
were administered; however, even with continuous high-dose
intravenous infusion of blood pressure-raising drugs, the patient
had recurring low blood pressure. Ten hours after resuscitation,
the blood pressure was maintained at 90–100/60–70 mmHg, and
small doses of dopamine (200 mg) and dobutamine (100 mg)
were continuously administered by a micro-pump.
Twelve hours after resuscitation, the patient’s blood pressure
remained stable. Fourteen hours after resuscitation, she developed
acute left ventricular failure and pink foamy sputum; the patient
was given medication for heart failure, including furosemide
dieresis and sodium nitroprusside.
Three days later, her vital signs gradually became stable. Chest
radiographs demonstrated increased and blurred lung markings
on both sides, a small shadow in the lung and no abnormalities
in the size, shape and position of the heart. The ECG results
demonstrated a small amount of pericardial effusion, reduced left
ventricular wall motion, mild mitral and tricuspid regurgitation
and an ejection fraction (EF) of 51%.
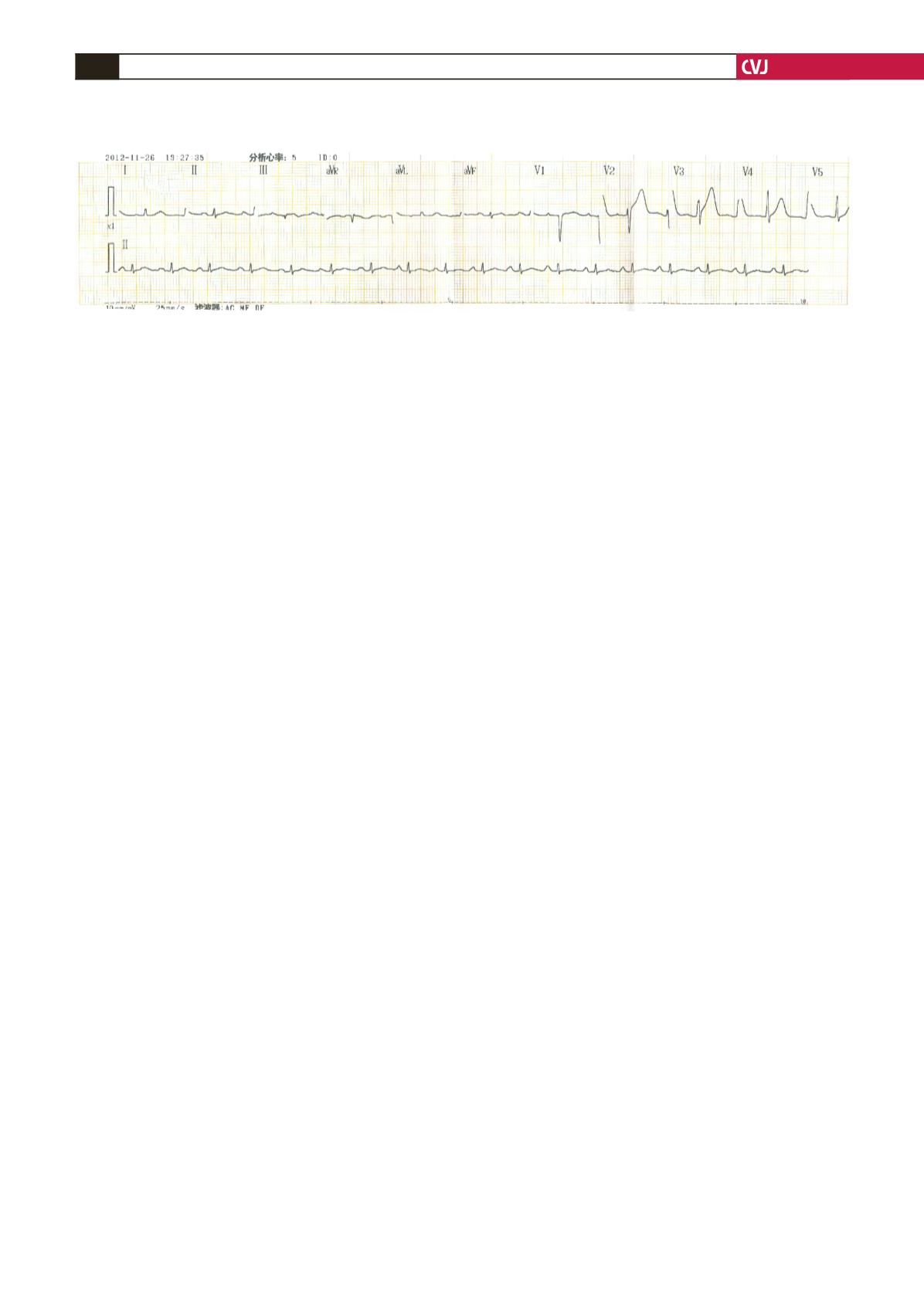
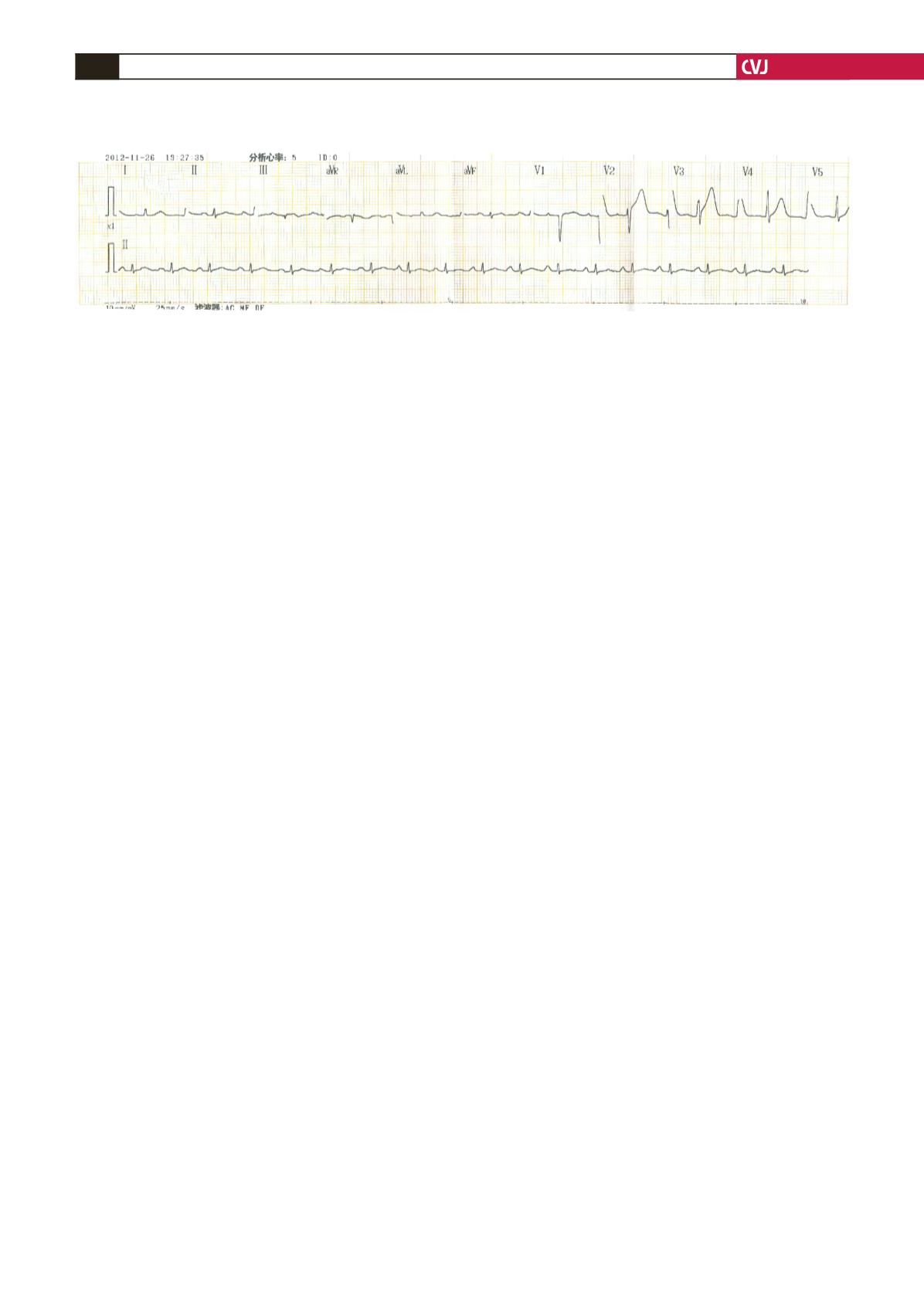
One week after hospitalisation, the patient experienced
paroxysmal chest pain three times, and each occurrence lasted
for five to 10 minutes. The pain was relieved with sublingual
nitroglycerin. An ECG during paroxysmal chest pain showed a
QS pattern in leads V1–V3; in leads V4–V6, an inverted T wave
became upright during the pain and returned to inverted when
the pain was relieved (Fig. 3). For treatment, aspirin, clopidogrel,
isosorbide mononitrate, rosuvastatin and trimetazidine were
administered.
Two weeks later, the patient’s condition stabilised. A coronary
angiograph displayed no significant abnormalities in the left main,
left anterior descending or circumflex arteries (Fig. 4), but a right
coronary spasm was visible (Fig. 4). Routine blood testing prior
to admission showed eosinophils at 0.52 × 10
9
/l, and this value
increased to 5.1 × 10
9
/l during hospitalisation and then dropped
to 0.53 × 10
9
/l prior to discharge. The patient’s immunoglobulin
E (IgE) was higher than 200 IU/ml, which indicated an increased
titre. However, no significant abnormalities were identified by
auto-antibody, anti-nuclear antibody, anti-dsDNA antibody or
anti-mitochondrial antibody tests. The high-sensitivity C-reactive
protein and immunoglobulin levels were normal. The patient’s
oestrogen and progesterone levels were within normal ranges.
Based on the previous medication plan, clopidogrel was
stopped, and diltiazem and trimetazidine were administered
instead. The patient was advised to stop taking progesterone
capsules. The discharge diagnosis was Kounis syndrome with
acute anterior myocardial infarction and cardiogenic shock
(Killip class IV). After discharge, the patient received long-
term medication to control the disease and remained in a stable
condition without paroxysmal chest pain. At the three-month
follow up, the patient’s menstrual cycle was regular and had a
reasonable amount of flow.
Discussion
Acute myocardial infarction primarily affects older men and
postmenopausal women; it is rare in young women. The patient
in this study was a slim young woman with no history of
smoking, alcohol abuse or other risk factors for coronary heart
disease, such as obesity, hyperlipidaemia, diabetes or high blood
pressure. There was no family history of coronary artery disease.
The patient had taken progesterone capsules every month prior
to the onset of chest pain and later developed recurrent chest
pain; therefore, we suspected that the unstable angina pectoris
was related to progesterone use. Myocardial infarction in female
patients has been correlated with hormone levels,
6
and chest pain
has been correlated with progesterone drugs.
7
The cause of the present patient’s cardiogenic shock was acute
myocardial infarction. Coronary angiography confirmed that the
cause of the acute anterior myocardial infarction was coronary
artery spasm and indicated a right coronary artery spasm and
normal left coronary and descending arteries.
7
However, the
presence of a left and right coronary spasm, which may have led
Fig. 3. An ECG during chest pain. Indication: sinus rhythm, old anterior myocardial infarction, hyper-acute T wave in
leads V4–V6.