CARDIOVASCULAR JOURNAL OF AFRICA • Volume 26, No 4, July/August 2015
AFRICA
e13
tenting length were 7.8 cm
2
and 1.8 cm, respectively. The mitral
annular dimension was 4.8 cm.
After spontaneous narrowing of the QRS duration to
60 ms, the third echocardiography showed mild MR with
improved pulmonary pressure (Fig. 2). Ischaemic heart disease
was excluded by coronary angiography. During follow up,
paroxysmal LBBB recurred repeatedly, all with pulmonary
oedema symptoms resolving with conversion to sinus rhythm
without LBBB.
Because of the severe symptoms, which were resistant to
medical therapy, we decided to perform mitral valve repair
surgery. Mitral valvuloplasty with a rigid annuloplasty ring (Sorin
Memo 3D 28-mm semi-rigid mitral) was performed. Within two
years following the procedure, the patient had no symptoms of
heart failure despite having paroxysmal LBBB attacks.
Case 2
A 56-year-old female had complained of exertional dyspnoea
and gradual intolerance during exercise for the previous three
months. Transthoracic echocardiography (TTE), which was
performed in another hospital, had revealed moderate-to-severe
mitral regurgitation and therefore she was referred to have
surgery for mitral valve replacement.
Her medical history was unremarkable for cardiovascular
disease and she was not taking any anti-arrhythmia drugs.
Initially, ECG revealed sinus rhythm with a heart rate of 66 bpm.
TTE showed normal chamber volumes and functions
with mild MR. During the TTE assessment she developed
sudden dyspnoea with 2:1 atrio-ventricular (AV) block, and
colour Doppler echocardiography revealed moderate early and
mid-diastolic mitral regurgitation jets (V
max
= 1.2 m/s, V–A
gradient of 6 mmHg) that regularly followed blocked P waves
(Fig. 3).
She was treated with a DDD pacemaker. No symptoms
occurred during one year of followup. Further TTE examinations
showed no diastolic mitral regurgitation.
Discussion
Competence of themitral valve requires a temporally and spatially
coordinated interaction of the mitral leaflets with the annulus,
chordae tendinae and papillary muscles. Dysfunction of any of
these components affects the normal systolic coaptation of the
anterior and posterior leaflets and causes mitral regurgitation.
Mechanistically, mitral regurgitation (MR) is classified as
either primary (intrinsic valve disease) or functional.
1
Functional
MR occurs in patients with a structurally normal valve (generally
with restricted leaflet mobility), mitral annular dilation, and left
ventricular remodelling.
2
Functional MR is further classified as
systolic and diastolic due to timing in the cardiac cycle.
Ischaemia is a well-known cause of functional MR.
3
The
underlying mechanism is apical tenting of structurally normal
leaflets with subsequent papillary muscle displacement away
from the mitral annulus plane.
4
Eclipsed mitral regurgitation
is an atypical form of sudden transient functional MR and is
reported as sudden apical tenting of both leaflets in the absence
of epicardial coronary artery stenosis and pre-existing LV
systolic dysfunction or remodelling.
5
Avierinos
et al
. reported severe mitral regurgitation with
symptoms of heart failure that was induced by methylergonovine
injection. Possible underlying mechanisms were epicardial focal
spasm, diffuse epicardial vasoconstriction or microvascular
dysfunction.
Rhythm and conduction disturbances are also common
causes of mitral regurgitation. Electromechanical asynchrony
can alter the left ventricular contraction pattern. Left bundle
branch block (as in our first case) is an example of ventricular
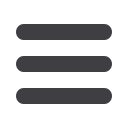
Fig. 2.
Transoesophageal echocardiography images demonstrating mild mitral regurgitation (panels A and B) with a 3.9-cm
2
tenting
area (panel C), and decreased pulmonary artery pressure to 40 mmHg (panel D). (RA: right atrium, RV: right ventricle, Ao:
aorta.)
A
C
B
D
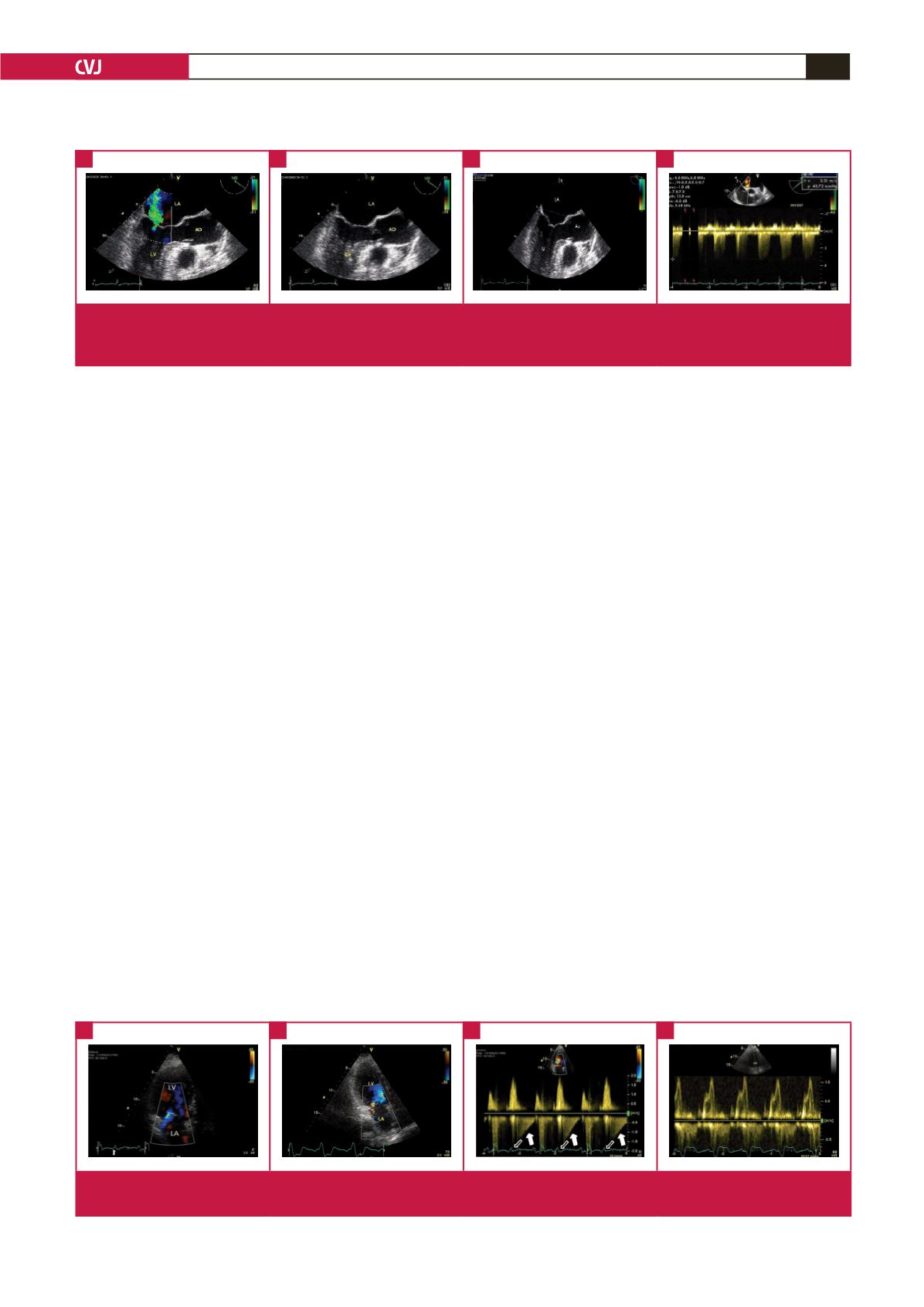
Fig. 3.
Colour (A) and continuous-flow Doppler (B) images demonstrating diastolic mitral regurgitation. The bold arrows represent
diastolic regurgitation; open arrows represent blocked P waves.
A
C
B
D

















