CARDIOVASCULAR JOURNAL OF AFRICA • Volume 26, No 4, July/August 2015
e12
AFRICA
Case Report
Intermittent symptomatic functional mitral regurgitation
illustrated by two cases
Alper Aydin, Tayfun Gurol, Ozer Soylu, Bahadir Dagdeviren
Abstract
Functional mitral regurgitation may have different haemo-
dynamic consequences, clinical implications and treatment
options, such as surgical or percutaneous interventions or
implanting a pacemaker. Here we present two cases with
haemodynamically significant intermittent functional mitral
regurgitation as the underlying mechanism of heart fail-
ure. The cases underline the importance of a high index of
suspicion in patients with intermittent heart failure, and a
careful analysis of echocardiographic images with simultane-
ous ECG, in order to delineate systolic and diastolic mitral
regurgitation.
Keywords:
mitral regurgitation, electromechanical delay, Doppler
echocardiography, left bundle branch block, mitral insufficiency
Submitted 24/4/13, accepted 25/2/15
Cardiovasc J Afr
2015;
26
: e12–e14
www.cvja.co.zaDOI: 10.5830/CVJA-2015-026
Heart failure (HF) in patients with normal left ventricular
ejection fraction accounts for half of the diagnoses of HF.
Careful echocardiographic analysis with simultaneous ECG in
two patients developing acute heart failure allowed identification
of an unusual cause of HF with normal left ventricular ejection
fraction (LVEF), but related to sudden reversible functional
mitral regurgitation in the absence of significant coronary artery
stenosis.
Case 1
A 54-year-old female was admitted to hospital with acute
pulmonary oedema. Her ECG showed sinus tachycardia with
left bundle branch block (LBBB) morphology, with a rate of
125 beats per min (bpm). Her symptoms improved following
spontaneous conversion to sinus rhythm without LBBB.
Two-dimensional echocardiography revealed concentric left
ventricular (LV) hypertrophy with normal systolic function
(LVEF 70%), with mild rheumatic mitral regurgitation (MR),
mild left atrial dilatation (4.3 cm) and elevated pulmonary artery
systolic pressure (50 mmHg). The tenting area of the mitral
leaflets and the tenting length was measured as 3.9 cm
2
and
1.3 cm, respectively. The mitral annular dimension was 4.2 cm.
The results of her laboratory examination were normal.
Her medical history was unremarkable for cardiovascular
disease and she was not taking any anti-arrhythmia drugs.
Since her symptoms occurred again the following day, the
echocardiographic examination was repeated. In the second
study, the rhythm was sinus tachycardia with LBBB morphology.
The QRS duration was 150 ms.
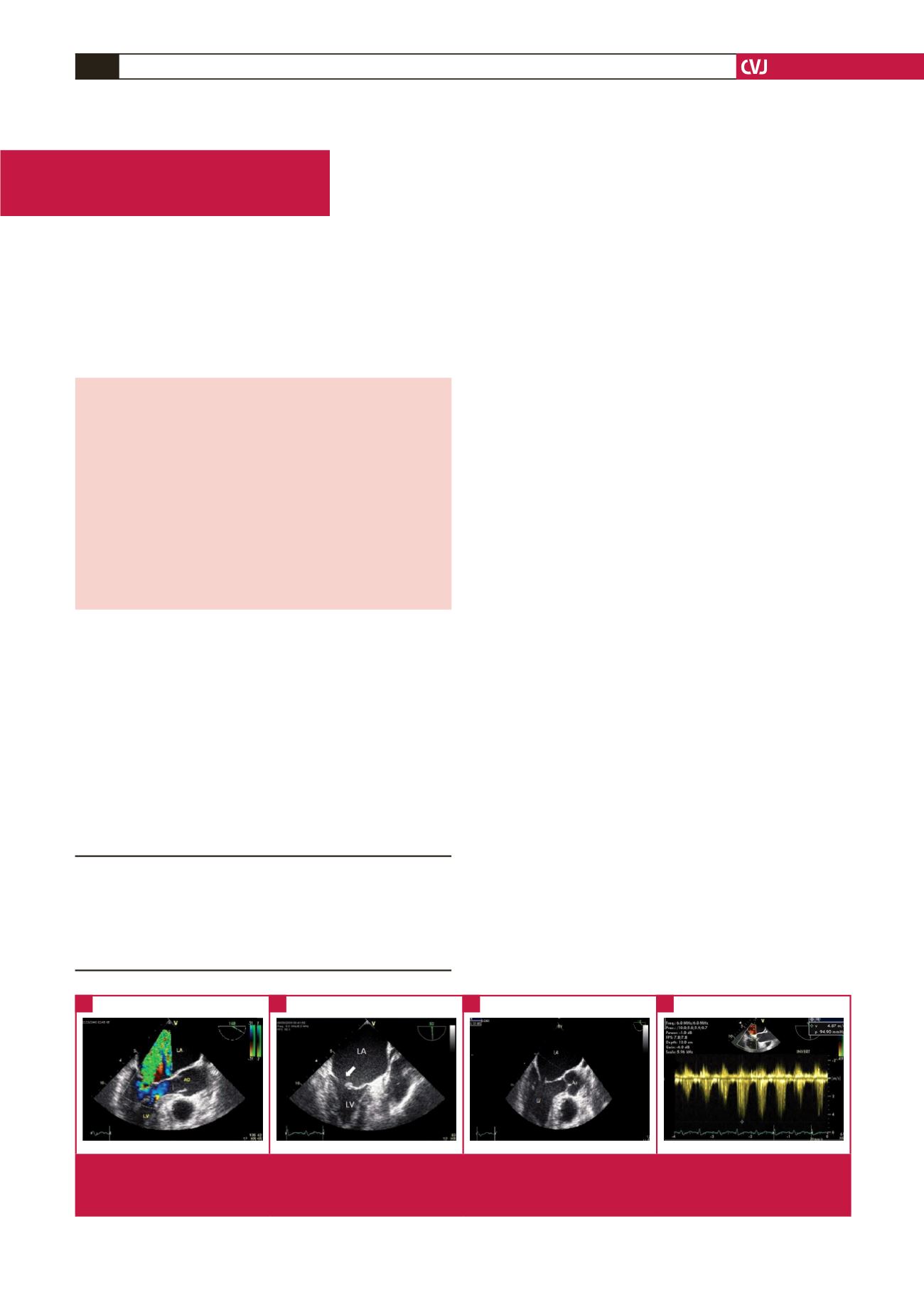
Transoesophageal echocardiography (TEE) revealed marked
asynchronous contraction and dilatation of the left ventricle
and atrium (5.1 cm). The left atrium was seen as being larger in
this second assessment (5.1 cm), with severe MR (Fig. 1). The
effective regurgitant orifice area was 0.6 cm
2
with a regurgitant
volume of 67 ml. The tenting area of the mitral leaflets and the
Department of Cardiology, Faculty of Medicine, Bahcesehir
University, Istanbul, Turkey
Alper Aydin, MD,
dralperaydin@gmail.comTayfun Gurol, MD
Ozer Soylu, MD
Bahadir Dagdeviren, MD
Fig. 1.
Transoesophageal echocardiography images demonstrating severe mitral regurgitation (A) during left bundle branch block.
The arrow in B shows impaired coaptation of the mitral valve leaflets (LA: left atrium, LV: left ventricle). The tenting area was
measured as 7.8 cm
2
(C), and the pulmonary artery pressure (D) was elevated to 95 mmHg.
A
C
B
D

















