CARDIOVASCULAR JOURNAL OF AFRICA • Volume 26, No 6, November/December 2015
AFRICA
211
Subjects using ophthalmic beta-blockers were selected and
followed for permanent pacemaker requirement during the
hospitalisation period and for three months after discontinuation
of the drug. Topical beta-blockers were discontinued after the
initial refererral to the hospital. According to the response of
the AV conduction after drug withdrawal, the type of adverse
drug reaction was identified from the definition of ‘adverse drug
reactions’ reported by Edwards and Aronson.
14
A permanent pacemaker was implanted in patients in whom
AV block persisted beyond 72 hours or recurred during the
follow-up period. All of the patients were referred to their
primary physicians for treatment of glaucoma after discharge.
Statistical analysis
All data were presented as mean
±
SD for parametric variables
and as percentages for categorical variables, unless stated
otherwise. Categorical variables were analysed with the Pearson’s
χ
2
test and Fisher’s exact test. All statistical studies were carried
out using Statistical Package for Social Sciences software (SPSS
16.0 for Windows, SPSS Inc, Chicago, Illinois) and a
p
-value
<
0.05 was considered statistically significant.
Results
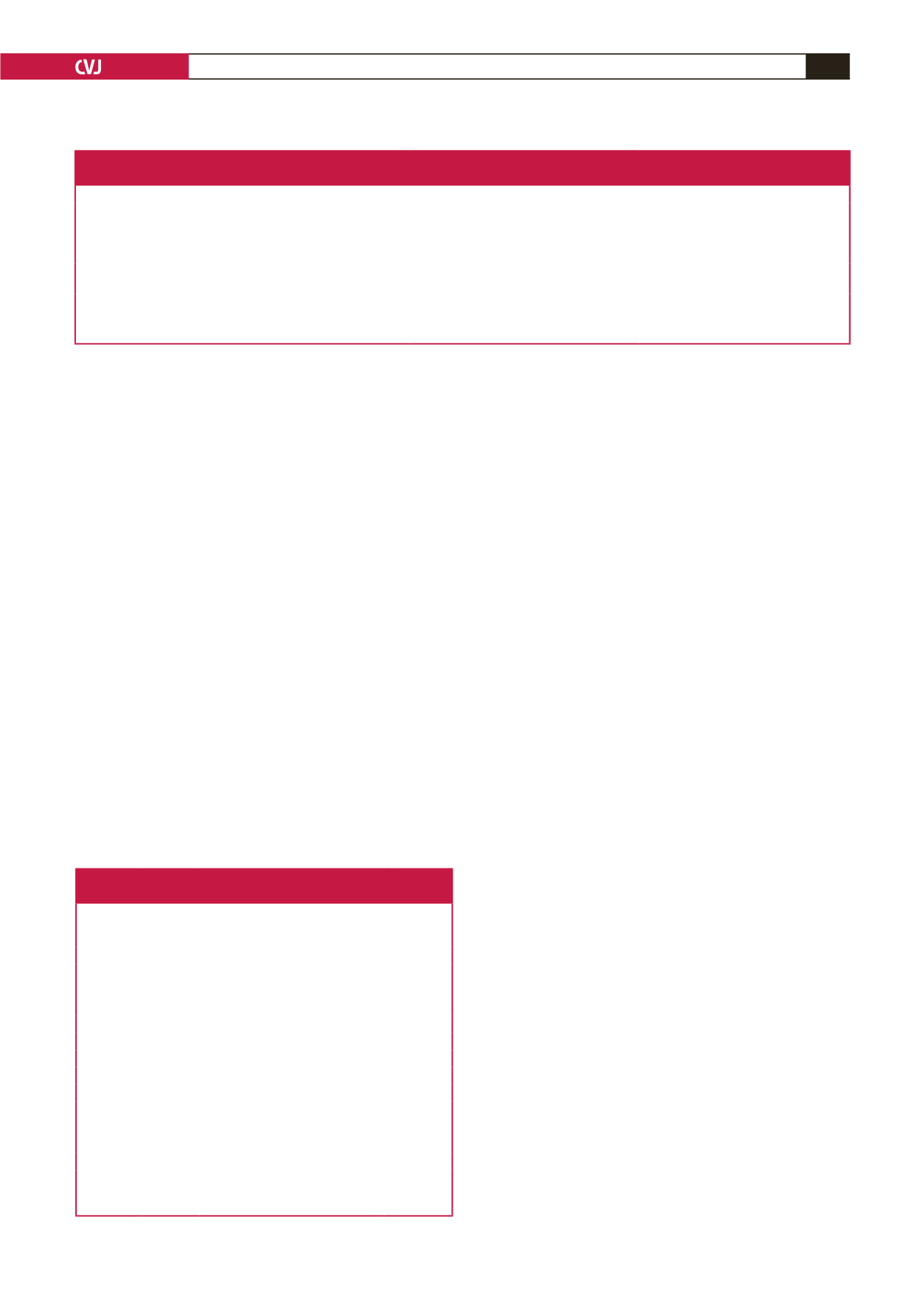
A total of 1 122 patients were hospitalised with a diagnosis of
AV block and a permanent pacemaker was implanted in 946
cases (84.3%). Thirteen of the 1 122 patients (1.1%) were using
ophthalmic beta-blockers for the treatment of glaucoma. The
demographic and clinical characteristics of these patients are
summarised in Table 2. None of these 13 patients were using
rate-limiting agents (oral beta-blockers, non-dihydropyridine
calcium channel blockers, digoxin and anti-arrhythmic drugs).
The mean age was 71.7
±
10.1 years and six patients in this
group were male (46%). Nine patients had hypertension (69%) and
four (30%) had coronary artery disease. The mean left ventricular
ejection fraction was 58.4
±
11.1% in the study population. The
major symptoms were syncope in five subjects, dizziness in four,
and bradyarrhythmia-related dyspnoea in four. The ophthalmic
beta-blocker used was timolol in seven cases (55%), betaxolol
in four (30%), and cartelol in two (15%). The mean duration of
ophthalmic beta-blocker treatment was 30.1
±
15.9 months.
On ECG, eight patients had complete AV block and five had
high-degree AV block. The level of conduction block, according
to ECG criteria, was as follows: four patients on betaxolol
(100%) had infra-nodal block; two on cartelol (100%) had
undetermined rhythm, four on timolol had infra-nodal block
(57%), and three (43%) on timolol had AV node block.
After drug discontinuation, in 10 patients the block persisted
and a permanent pacemaker was implanted. Three patients (two
on timolol and one on cartelol therapy), in whom the AV block had
resolved, were discharged without pacemaker implantation. In one
patient on previous cartelol treatment, the AV block reccurred one
month after hospital discharge and a permanent pacemaker was
implanted. Therefore, in total, 11 of 13 patients required permanent
pacemaker implantation (84.6%). The implantation rate did not
differ according to the type of topical beta-blocker used (
p
=
0.37).
The distribution of ophthalmic beta-blockers in those who
required permanent pacemaker implantation were timolol in
five cases, betaxolol in four, and cartelol in two cases. The
level of conduction block in patients who required permanent
pacemaker implantation were infra-nodal block in eight cases,
AV node block in one case and undetermined level of block in
two cases. Only two patients on timolol therapy, whose ECGs
were compatible with AV node block, did not require pacemaker
implantation. On the other hand, all of the subjects with infra-
nodal block on ECG required pacemaker implantation.
Discussion
Drug-induced AV block is not a well-known clinical entity and
there are controversial reports in the literature.
15,16
Moreover,
little is known about the natural history and prognosis of
patients with drug-induced AV block on treatment with topical
beta-blockers. The main finding of our study was that most of
Table 1. Classification of second- and third-degree AV block, and atrial fibrillation with bradyarrhythmia,
based on electrocardiographic characteristics
AV nodal block
Infra-nodal AV block
Undetermined level of AV block
Second-degree
AV block
PR increment preceding a blocked P
(Wenckebach) and narrow QRS
Constant PR interval preceding blocked P PR increment (Wenckebach) preceding a
blocked P and wide QRS
2:1 AV block
Conducted impulse has long PR and
narrow QRS; PR varies inversely with RP
Conducted impulse has normal PR and wide
QRS; PR is constant despite varying RP
Conducted impulse has long PR and
wide QRS or short PR and narrow QRS
Third-degree
AV block
Escape rhythm has narrow QRS and rate
≥ 40 beats/min
Escape rhythm has wide QRS and rate
<
40 beats/min
Escape rhythm has wide QRS and rate
≥ 40 beats/min
Atrial fibrillation and
bradyarrhythmia
f waves with irregular narrow QRS
f waves with regular wide QRS
f waves with irregular wide QRS
AV
=
atrioventricular.
Table 2. Characteristics of patients with ophtalmic
beta-blocker-induced conduction defects
Patient’s
age/gender Drug type
Therapy
duration
(months) Conduction defect
Temporary/
permanent
pacemeker
81/M Betaxolol
24
3rd-degree AV block Yes/Yes
58/F
Timolol
40
Sinus pause
No/Yes
78/F
Timolol
52
3rd-degree AV block Yes/No*
82/M Timolol
14
High-degree AV block No/Yes
85/M Timolol
15
3rd-degree AV block No/Yes
62/F
Timolol
61
Sinus pause
No/No*
56/F
Timolol
44
3rd-degree AV block No/Yes
62/M Cartelol
32
High-degree AV block No/Yes**
73/M Betaxolol
16
3rd-degree AV block No/Yes
83/F
Betaxolol
18
High-degree AV block No/Yes
72/M Cartelol
11
3rd-degree AV block Yes/Yes
65/F
Betaxolol
37
High-degree AV block No/Yes
76/M Timolol
27
3rd-degree AV block No/Yes
*Rhythm was improved and conduction disturbance never recurred after
drug withdrawal; **Rhythm was improved but recurred one month after
drug discontinuation. AV: atrioventricular.

















