CARDIOVASCULAR JOURNAL OF AFRICA • Volume 26, No 6, November/December 2015
206
AFRICA
Results
In total, 48 patients were included in the study. The demographic
and clinical characteristics of the patients are given in Table
1. The mean time of admission was 5.2 (2–10) hours. While
ST-segment depression was seen on the ECG of 14 patients
(29%), T-wave negativity was seen in 20 (42%) and ST–T segment
changes were not detected in 14 patients (29%). A diagnosis
of NSTEMI was made in 24 out of 48 patients. Coronary
angiography was performed in 40 patients.
While H-FABP assessment on admission (two to 10 hours
after onset of chest pain) was positive in 20 out of 24 patients
whose NSTEMI diagnoses were definite, negative results were
obtained in four patients. These four patients constituted the
false-negative patient group. H-FABP was found to be negative
in 22 out of 24 patients in whom NSTEMI was eliminated,
and it was found to be positive in two. These two patients
constituted the false-positive patient group. Table 2 summarises
the positivity and negativity of the cardiac markers, which were
tested on admission. The results of the analyses based on these
data showed that diagnostic sensitivity was 83.3%, specificity was
91.7%, NPV was 84.6%, PPV was 90.6%, and AI was 87% for
H-FABP in the diagnosis of NSTEMI.
Comparisons of these values with other cardiac markers
are summarised in Table 3. A comparative analysis of the data
obtained when the patients were divided into three groups,
according to admission times (
≤
three hours, three to six hours,
and
>
six hours after onset of symptoms) is given in Table 4, and
two groups (
≤
six hours and
>
six hours after onset of symptoms)
is given in Table 5. The sensitivity and specificity of H-FABP for
≤
three hours were calculated as 89 and 100%, respectively, the
sensitivity and specificity for three to six hours were 70 and 89%,
respectively, and the sensitivity and specificity for
>
six hours
were 100 and 89%, respectively.
The respective sensitivities of bedside H-FABP and tnI tests
were 89 vs 33% (
p
<
0.05) for patients presenting within three
hours of onset. When H-FABP, CK-MB and TnI were compared
according to AI at
≤
three and three to six hours, H-FABP was
shown to be a better diagnostic marker (
p
<
0.01 and
p
<
0.05,
respectively).
From the assessment of the two groups of admission times
(
≤
six hours and
>
six hours after onset of symptoms), the
diagnostic sensitivity and specificity of H-FABP levels were
found to be 79 and 93% for
≤
six hours, respectively, while
sensitivity and specificity were found to be 100 and 89% for
>
six hours, respectively. These values indicate that H-FABP is a
sensitive and specific marker for the diagnosis of NSTEMI at
≤
six hours (accuracy 85%).
When AI values were compared, H-FABP was found to be
a better diagnostic marker than TnI (85 vs 65%,
p
<
0.05) and
CK-MB (85 vs 62%,
p
<
0.05) for the early period (
≤
six hours).
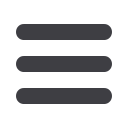
Table 1. Patients’ characteristics
Characteristic
Number (%) or mean ± SD
(minimum
–
maximum values)
Age
60 ± 9 (38–79)
Male gender
28 (58)
Hypertension
35 (73)
Diabetes mellitus
14 (29)
Smoking
23 (48)
Total cholesterol (mg/dl)
204 ± 57 (97–311)
(mmol/l)
5.28 ± 1.48 (2.51–8.05)
LDL-C (mg/dl)
124 ± 55 (34–243)
(mmol/l)
3.21 ± 1.42 (0.88–6.29)
HDL-C (mg/dl)
45 ± 11 (14–69)
(mmol/l)
1.17 ± 0.28 (0.36–1.79)
Triglycerides (mg/dl)
148 ± 88 (19–533)
(mmol/l)
1.67 ± 0.99 (0.21–6.02)
Family history
12 (25)
History of CAD
15 (31)
Admission time (hours)
5.2 ± 2.4 (2–10)
ECG on admission
ST depression
14 (29)
T negativity
20 (42)
No ECG changes
14 (29)
Coronary angiography findings
Normal coronary arteries
7 (17.5)
Insignificant stenosis (
<
50%)
9 (22.5)
Single-vessel disease
13 (32.5)
Multiple-vessel disease
11 (27.5)
LDL-C, low-density lipoprotein cholesterol; HDL-C, high-density
lipoprotein cholesterol; CAD, coronary artery disease.
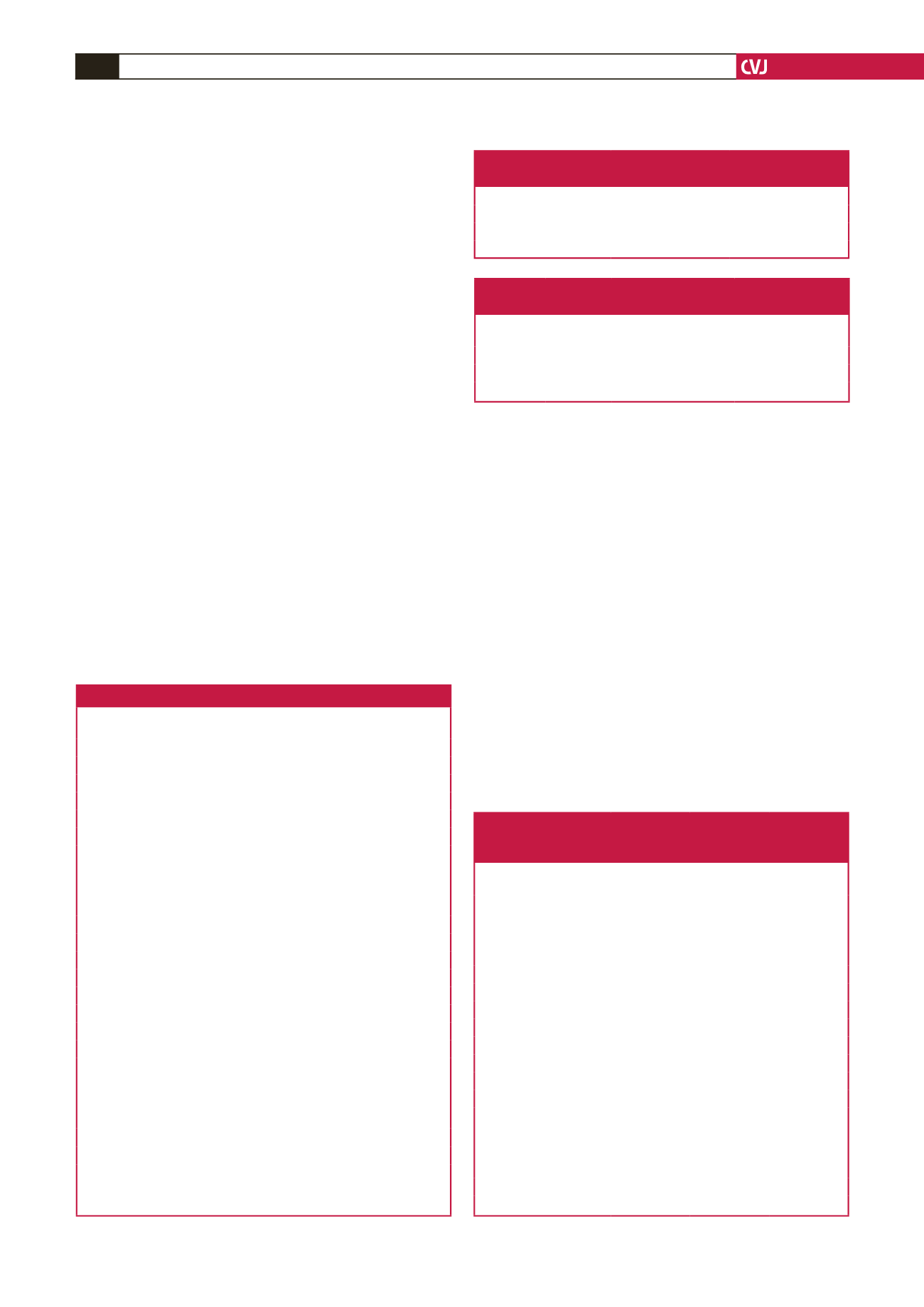
Table 2. Cardiac markers of the patients who were
diagnosed with and without NSTEMI
NSTEMI + (
n
=
24) NSTEMI
–
(
n
=
24)
H-FABP positive,
n
(%)
20 (83.3)
2 (8.3)
TnI positive,
n
(%)
15 (62.5)
4 (16.6)
CK-MB positive,
n
(%)
12 (50)
1 (4.1)
Table 3. Sensitivity, specificity, NPV, PPV and AI of H-FABP,
TnI and CK-MB in the diagnosis of NSTEMI
Sensitivity
(%)
Specificity
(%)
NPV PPV AI
H-FABP
83.3
91.7
84.6
90.9
87.5
TnI
62.5
83.3
68.9
78.9
72.9
CK-MB
50
95.8
65.7
92.3
72.9
Table 4. Diagnostic value of H-FABP, TnI and CK-MB in
NSTEMI diagnosis, according to admission time after
onset of symptoms (
≤
3, 3–6 and
>
6 hours)
≤
3 hours
(
n
=
15)
3–6 hours
(
n
=
19)
>
6 hours
(
n
=
14)
H-FABP
Sensitivity (%)
89
70
100
Specificity (%)
100
89
89
NPV (%)
86
73
100
PPV (%)
100
88
83
AI (%)
93
78
92
TnI
Sensitivity (%)
33
70
100
Specificity (%)
100
67
89
NPV (%)
50
67
100
PPV (%)
100
70
83
AI (%)
60
68
92
CK-MB mass
Sensitivity (%)
22
50
100
Specificity (%)
100
89
100
NPV (%)
46
62
100
PPV (%)
100
83
100
AI (%)
53
68
100

















