CARDIOVASCULAR JOURNAL OF AFRICA • Volume 30, No 5, September/October 2019
AFRICA
255
patients with constrictive pericarditis out of a sample size of
3 847 undergoing pericardiectomy.
In keepingwith other studies fromdeveloping countries,
2,11,12,19-21
and in contrast to Western series,
22,23
tuberculosis was the
major aetiology of constrictive pericarditis in our study and
highlights the impact of the HIV/AIDS epidemic in refuelling a
resurgence of tuberculosis infections.
24,25
Similar to other series,
2,15
proven tuberculosis (pericardial histology, culture of AFB from
sputum, lymph nodes) was documented in 22 (26.5%) of the
patients. In contrast to Reuter’s findings in TB pericarditis,
26
we
found histological evidence of definite tuberculosis in only nine
operative pericardial biopsy specimens and could not determine
from these small numbers whether histological evidence of
tuberculosis is more common in HIV-positive subjects. The
natural history of tuberculous pericarditis has been previously
described, including treatment options to prevent progression to
constriction.
16,27-30
In this study we found few differences in the clinical profile
between HIV-positive and -negative patients. The higher levels
of alkaline phosphatase and gamma glutamyl transferase among
HIV-positive patients might have been due to hepatic tuberculosis
or more likely to more severe hepatic congestion in these subjects.
Importantly, there was no difference in the pre-operative and
follow-up ejection fraction between HIV-positive and -negative
patients. This finding differs from studies in patients with
tuberculous pericarditis co-infected with HIV who have been
found to have a higher prevalence of myopericarditis.
27,31
Preservation of ejection fraction might explain why we
found no significant differences in peri-operative mortality
rate observed between HIV-positive and -negative patients. It
is also likely that antiretroviral therapy in our patients may
have helped to preserve left ventricular function by preventing
the development of opportunistic infections or HIV-associated
myocardial dysfunction.
Pericardial calcification was identified on chest radiography
in 17 (20.5%) of our study patients, which is much higher than
the 5% reported by Strang
et al
. in the pre-HIV era.
19
While
equivalent rates of pericardial calcification in HIV-positive and
-negative patients (21.4 vs 20.7%;
p
=
0.953) have been described
in the study by Mutyaba
et al
.,
2
we found that calcification was an
uncommon finding in HIV-positive compared with HIV-negative
patients (6.3 vs 29.4%;
p
=
0.011). Furthermore none of the eight
patients with CD4 counts
<
200 cells/mm
3
developed pericardial
calcification.
We attributed the higher prevalence of pericardial calcification
among HIV-negative patients to longer survival in these patients
with a more prolonged duration of infection, progressing to
fibrosis and calcification. Alternatively it could be explained by
the suppression of CD4 helper by the HI virus, leading to less
fibrogenesis and calcification in these subjects.
26
Among the 31 subjects who did not undergo early surgery,
15 patients on telephonic contact were still alive, and of these,
five reported improvement in their symptoms (survival status
unknown in two) on anti-tuberculous therapy. Strang
et al
.
32
have shown that a significant number of patients diagnosed with
tuberculous constrictive pericarditis may undergo resolution
of their symptoms on anti-tuberculous therapy. The high
pre-operative mortality rate of 16.78% in our study emphasises the
importance of pericardiectomy in ensuring a successful outcome
in subjects who do not respond to anti-tuberculous therapy.
Our analysis of the pre-operative outcome showed that
HIV status had no effect on the pre-operative mortality rate
in constrictive pericarditis in subjects on antiretroviral therapy.
Instead, our analysis showed that older age, unsuppressed viral
load, lower serum haemoglobin and albumin levels, as well as
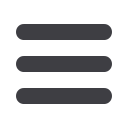
Six-week post-operative
NYHA class
Pre-operative NYHA class
NYHA I
n
=
3
NYHA I
n
=
33
2
21
NYHA II
n
=
9
NYHA II
n
=
53
6
10
NYHA III
n
=
22
NYHA III
n
=
0
1
NYHA IV
n
=
0
NYHA IV
n
=
5
1
1
Fig. 2.
Comparison of pre-operative and six-week postop-
erative New York Heart Association functional class
status in 41 patients (
p
<
0.0001). Most subjects
improved by at least one functional class. NYHA, New
York Heart Association.
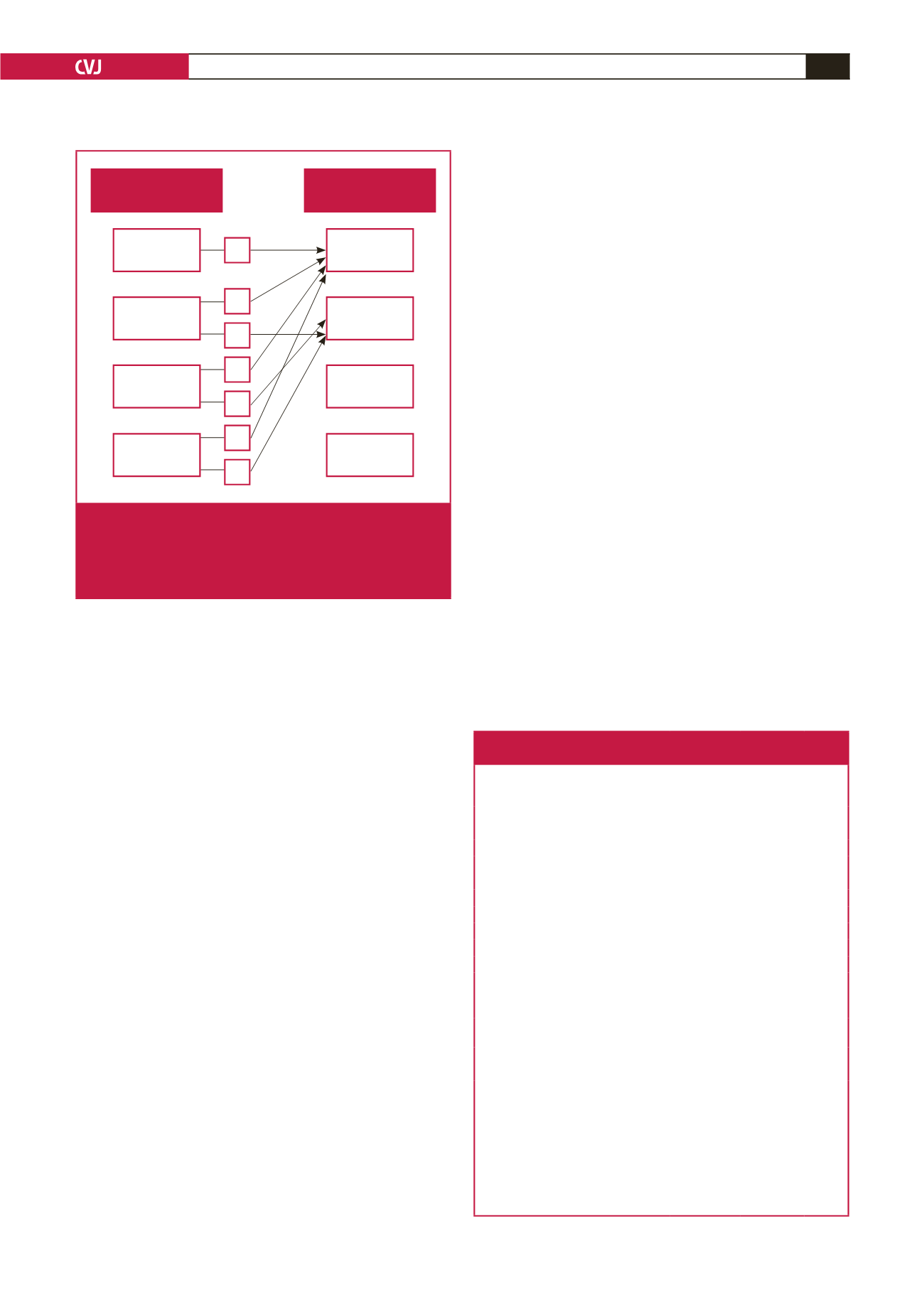
Table 3. Operative characteristics of study patients stratified
by HIV status
Characteristic
All (
n
=
52)
HIV
negative
(
n
=
32)
HIV
positive
(
n
=
20)
p-
value
Pericardiectomy
0.093
Total
38 (73.1)
26 (81.3)
12 (60.0)
Sub-total
9 (17.3)
2 (6.3)
7 (35.0)
Not known
5 (9.6)
4 (12.5)
1 (5.0)
Inotrope usage
48 (94.1)
31 (96.9)
17(85.0)
0.547
Days in ICU
4.59
±
2.84 4.28
±
2.74 5.11
±
2.84 0.321
Postoperative complications 15 (28.9)
6 (18.8)
9 (45.0)
0.030
Pericardial histology
Granulomas
9 (18.4)
4 (12.9)
5 (27.8)
0.259
Acid-fast bacilli
3 (6.1)
1 (3.2)
2 (11.1)
0.546
Calcification
12 (24.4)
10 (32.3)
2/18 (11.1) 0.168
Postoperative ejection
fraction
53.55
±
6.65 53.33
±
6.70 53.93
±
6.79 0.783
Postoperative six-week
follow up
0.687
NYHA l
33 (80.4)
20 (76.9)
13 (86.7)
NYHA ll
9 (21.4)
6 (23.1)
2 (18.8)
Ejection fraction
53
±
9.16 52.44
±
11.50 53.83
±
4.67 0.785
Data presented as mean
±
standard deviation for continuous variables and
n
(%)
for categorical variables.
ICU, intensive care unit; NYHA, New York Heart Association.
Details of inotrope usage was not available for one subject; three subjects’
histology results were not found (one HIV negative, two HIV positive); nine
subjects did not have postoperative measurement of ejection fraction (four HIV-
negative subjects and five HIV-positive subjects); 41 patients attended six-week
follow up (26 HIV negative, 15 HIV positive). Follow up ejection fraction (10
HIV-negative, five HIV-positive patients).



















