CARDIOVASCULAR JOURNAL OF AFRICA • Volume 30, No 1, January/February 2019
12
AFRICA
Multivariate analyses were performed in order to determine
the clinical and echocardiographic parameters that were
independently associated with PASP in the study population
(Table 6). A model was derived by forward stepwise multiple
linear regression analysis with PASP as the dependent variable.
The independent/predictor variables included in the analysis were
relevant clinical and left heart echocardiographic parameters with
statistically significant correlations on univariate analysis with
p
-values
<
0.05. These were age, gender, pulse rate, BMI, LAVI,
LV mass, LVEF, E/e
′
ratio and mitral regurgitant volume. Right
heart echo parameters were not included in the models because
they can be deranged as a consequence of PH and therefore are
not predisposing factors. The analysis revealed that only LAVI
and E/e
′
ratio were independently associated with PASP.
Discussion
This study showed that pulmonary hypertension was fairly
common among the HF subjects and was significantly
associated with clinical and echo indices of worsening HF
severity. The frequency of PH varies widely in the literature,
with a reported range of 7–83%.
1,2,5,14-22
This is likely due to
differences in assessment methods and cut-off values. We found
a PH frequency of 38.8%, which is quite close to that of some
studies
17,18
that employed a similar cut-off value but much lower
than in two community studies
1,2
carried out in the USA. Our
reported PH frequency is also lower than in two earlier local
studies done in Nigeria by Karaye
et al
.
14
and Amadi
et al
.,
22
reporting an occurrence of 66 and 70.4%, respectively. This
was probably due to the differences in PH estimation methods
employed.
The clinical characteristics of the HF subjects with and
without PH were compared. Significant differences were noted
with gender, BMI, pulse rate, systolic blood pressure and NYHA
functional class. The PH group in this study had a significantly
lower BMI than the non-PH group. This finding was also
reported by some investigators,
2,6
although other studies
1,5
did
not find any significant difference. A lower BMI in HF has
been associated with increased disease severity and higher
mortality risk, most likely due to the effects of TNF-alpha and
catecholamine excess, which lead to cachexia and depressed LV
function.
23,24
Therefore HF patients with a lower BMI are likely
to have poorer LV function and higher LV filling pressures,
which are associated with elevated PASP. This finding differs
from what is described in the normal population, where subjects
with higher BMI have slightly higher PASP.
25
In this study, a significantly higher proportion of the HF
subjects with PH were in NYHA class III and IV, compared
with the non-PH subgroup. This suggests that PH in HF patients
is associated with worsening HF severity, which has also been
reported by other studies.
2,5
This is an expected finding, bearing
in mind that decompensated HF patients usually present with an
increased level of pulmonary venous congestion as a result of
higher LV filling pressures.
3,4,26,27
A comparison of HF aetiologies between subjects with
and without PH was done in this study. Significant differences
were observed in the occurrence of hypertensive heart disease,
idiopathic dilated cardiomyopathy (DCM), and valvular
heart disease (VHD). The PH group had a significantly lower
frequency of hypertensive heart disease (37.6%) compared
with the non-PH group (56%). This was also reported
among hospitalised HF patients in a study done in northern
Nigeria.
14
In our study, PH was associated with a HF aetiology of
DCM and VHD. Amadi
et al
.
22
found a similar association
Table 5. Correlation between selected clinical and echo parameters
with estimated pulmonary artery systolic pressure
PASP
Parameters
r
p
-value
Clinical variables
Age
–0.163
0.02
BMI
–0.298
<
0.001
Pulse
0.138
0.04
SBP
–0.105
0.12
DBP
0.083
0.22
Previous admissions
0.037
†
0.59
Duration of HF
–0.048
†
0.51
Echocardiographic variables
LV diastolic diameter
0.237
0.002
LV systolic diameter
0.229
0.003
LV ejection fraction
–0.239
<
0.001
Fractional shortening
–0.240
<
0.001
LA volume index
0.565
<
0.001
LV mass index
0.269
<
0.001
TAPSE
–0.428
<
0.001
RV wall thickness
0.267
<
0.001
RV basal diameter
0.472
<
0.001
Right atrial area
0.550
<
0.001
Eccentricity index
0.481
<
0.001
E/e
′
ratio
0.415
<
0.001
Mitral regurgitant volume
0.269
<
0.001
†
Spearman’s ranked correlation coefficient.
r,
Pearson’s correlation coefficient; BMI, body mass index; SBP, systolic blood
pressure; DBP, diastolic blood pressure; LA, left atrium; LV, left ventricle;
TAPSE, tricuspid annular plane systolic excursion; RV, right ventricle; E, early
mitral inflow velocity; e’, early mitral annular diastolic velocity.
Table 6. Stepwise multivariate linear regression model identifying
determinants of estimated pulmonary artery systolic pressure
Variables
Standardised
β
-coefficient
p-
value
Model with PASP as dependent variable
Left atrial volume index
0.432
<
0.001
E/e
′
ratio
0.188
0.006
R
2
=
0.288
PASP, pulmonary artery systolic pressure; mPAP, mean pulmonary artery pres-
sure; E, mitral inflow E velocity; e
′
, early mitral annular diastolic velocity; R
2
,
coefficient of determination.
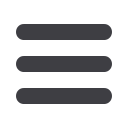
None
Grade 1
Grade 2
Grade 3
Percent
90
80
70
60
50
40
30
20
10
0
PH group (PASP > 36 mmHg)
non-PH group
Fig. 2.
Diastolic dysfunctional grade in the PH and non-PH
subgroups.

















