CARDIOVASCULAR JOURNAL OF AFRICA • Volume 30, No 1, January/February 2019
AFRICA
17
in urban areas. All physicians reported adhering to dyslipidaemia
guidelines: 57.9% to ESC/EAS, 31.6% to ACC/AHA and 5.3%
to other international guidelines. In addition, 42.1% stated that
they adhered to the local South African guidelines, which are
closely aligned with the ESC/EAS guidelines. Statin intolerance
was defined as intolerance to one, two or three statins by 15.8,
47.4 and 36.8% of physicians, respectively.
Of 427 patients assessed, 31 were ineligible for enrolment
(Fig. 1). Therefore, the study population comprised 396
patients (mean
±
SD age, 60.0
±
10.2 years; 56.3% men) (Table
1). Patient demographic and clinical characteristics, lipid values
and LMTs are shown according to cardiovascular risk level in
Tables 1 and 2.
Overall, 36.4% were Caucasian/European, 24.7% were Asian
(including South Asian) and 24.2% were black African. Most
(
n
=
367, 92.7%) patients were from urban/suburban areas, and
81.1% (
n
=
317) had completed secondary education or higher.
A total of 279 (70.5%) patients had private medical insurance.
Most patients (81.8%) had healthcare cover (public or private)
that included drug reimbursement (private medical insurance) or
drug supply (public sector).
Most (87.1%) were overweight or obese [defined as a
body mass index (BMI) of 25 to
<
30 kg/m
2
and
≥
30 kg/
m
2
, respectively], 57.3% were physically inactive, 53.9% had
the metabolic syndrome (Adult Treatment Panel III), 13.4%
were current smokers and 22.0% reported regular alcohol
consumption. Diabetes mellitus was present in 65.2% and
hypertension in 81.3% of patients. A total of 135 (34.1%) patients
had documented CAD: previous acute coronary syndrome
(88/135, 65.2%), percutaneous coronary intervention (75/135,
55.6%) or coronary artery bypass graft surgery (57/135, 42.2%).
Median time since dyslipidaemia diagnosis was 6.0
(interquartile range 3.0–12.0) years. The LDL-C value at the
time of first diagnosis was available in 130 (32.8%) patients;
mean untreated LDL-C was 3.9
±
1.4 mmol/l (151.7
±
52.7
mg/dl) and the LDL-C range was 0.7–9.0 mmol/l (27.0–347.5
mg/dl). At first diagnosis, 63.8% (83/130) of patients had an
LDL-C value
>
3.4 mmol/l (130 mg/dl) and 18.5% (24/130) had
LDL-C
>
4.9 mmol/l (190 mg/dl). Definite or probable familial
hypercholesterolaemia was reported in 6.2% of patients.
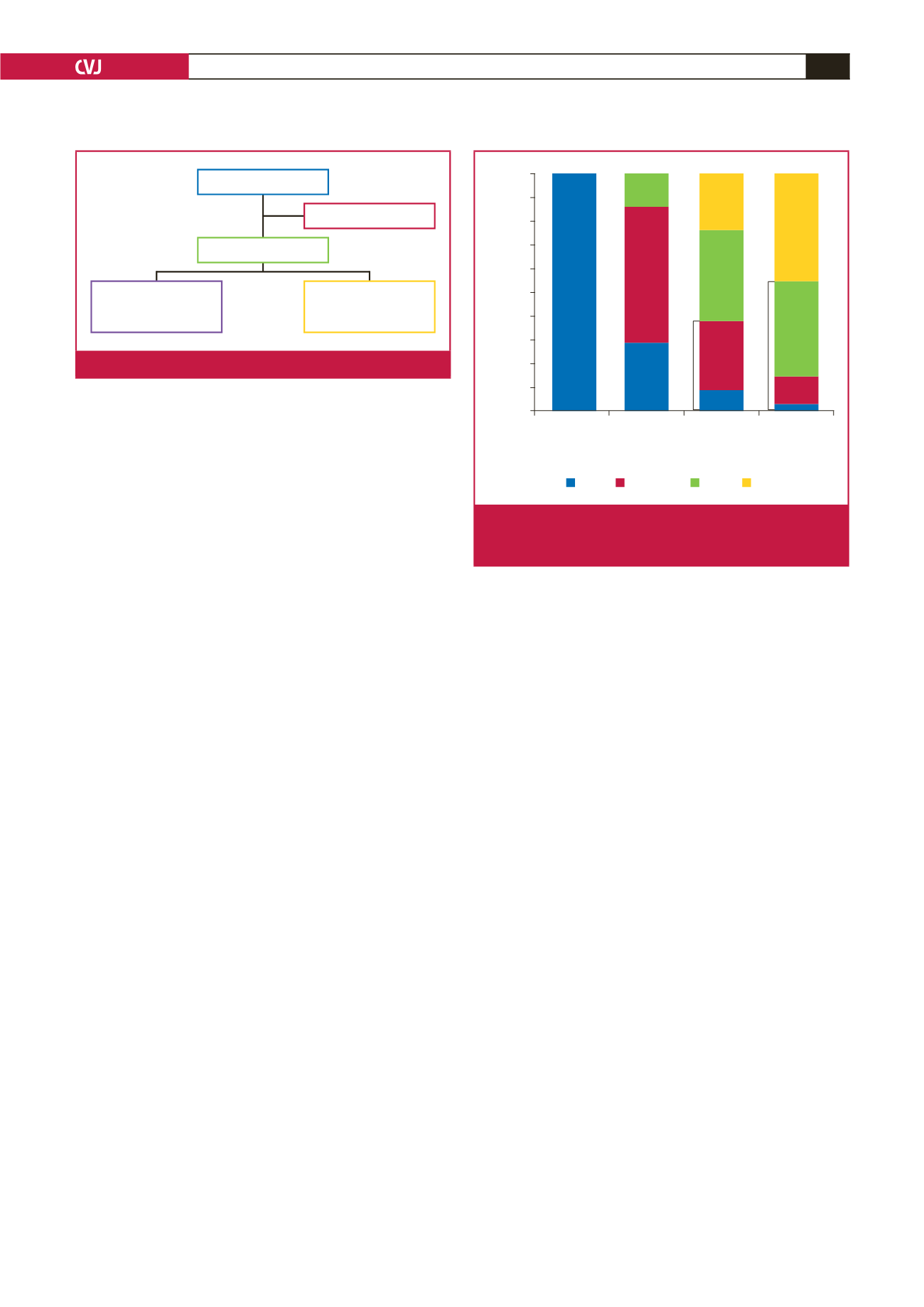
Of the 354 (89.4%) patients in whom SCORE cardiovascular
risk could be calculated, 63.0% were at very high risk, 34.7% at
high risk, 2.0% at moderate risk and 0.3% (one patient) was at low
risk. Physician-estimated risk correlated poorly with calculated
risk (Fig. 2); physicians underestimated risk in 54.7% of patients
at very high calculated risk and 38.2% of those at high risk.
Tables 3 and 4 show patient demographic and clinical
characteristics, lipid values and LMTs by patient ethnicity. A
smaller proportion of black African patients were male (35.4%)
compared with other ethnic groups (53.4–72.2%). In the black
African patient group, the incidences of obesity and hypertension
were 63.5 and 89.6%, respectively. Corresponding figures in the
other ethnic groups ranged from 32.7 to 54.2% for obesity and
71.5 to 87.9% for hypertension. Rates of documented CAD were
10.4% in black Africans compared with 28.6 to 50.0% in other
ethnic groups.
At study enrolment, 98.7% of patients were receiving statin
therapy; 90.7% were receiving statin monotherapy, 3.3% were
receiving statin plus a fibrate, and 2.6% were receiving a statin
plus a cholesterol-absorption inhibitor (Table 1). One-quarter of
patients treated with statins were receiving high-intensity statin
therapy (that is, atorvastatin 40 or 80 mg, or rosuvastatin 20 or
40 mg) and 17.7% were on the highest-dose regimen available in
South Africa at the time of the study.
Mean LDL-C value at enrolment was 2.6
±
1.0 mmol/l
(98.7
±
39.6 mg/dl) (Table 2). Overall, 41.4% of patients were
at or below their LDL-C target at enrolment (Figs 3A and 4).
Among patients for whom SCORE cardiovascular risk could
be assessed, achievement rates were 14.3, 59.3 and 32.3% for
those at moderate, high and very high risk, respectively (Fig.
3A). Around half of Asian (54.7%) and black African (53.2%)
patients achieved their LDL-C target compared with 29.8% of
European/Caucasian patients and 27.3% of patients of ‘other’
ethnicity (Fig. 3B); achievement rates ranged from 65.0% in
patients seen by physicians with several specialities to 6.3% in
patients under the care of a cardiologist (Fig. 3C).
Discussion
This observational study in patients on stable LMT indicated
that achievement of LDL-C goals in South Africa is inadequate,
427 patients screened
396 patients enrolled
354 (89.4%) patients
cardiovascular risk
assessable
42 (10.6%) patients
cardiovascular risk
not assessable
31 patients ineligible
Fig. 1.
Patient flow chart.
Calculated cardiovascular risk level (SCORE)
Low
(
n
=
1)
Moderate
(
n
=
7)
High
(
n
=
123)
Very high
(
n
=
223)
Physician-estimated cardiovascular risk (%)
100
90
80
70
60
50
40
30
20
10
0
100
28.6
8.9
29.3
57.1
38.2
14.2
23.6
45.3
40.4
38.2
Very high
High
54.7
11.7
2.7
Moderate
Low
Fig. 2.
Physician-estimated assessment of patient cardio-
vascular risk versus calculated risk (calculated using
SCORE
16
).

















