CARDIOVASCULAR JOURNAL OF AFRICA • Volume 30, No 1, January/February 2019
AFRICA
21
foods, which may have contributed to a rise in cardiovascular
risk factors relative to other ethnic groups. Despite the lower
level of education and private health cover, and high rates of
cardiovascular risk factors in black African patients, LDL-C
target attainment rate was 53.2% in this group compared with
54.7% in Asians and 29.8% in Caucasian/Europeans.
Better LDL-C target achievement in black African patients
may partially be due to the high prevalence of diabetes mellitus
in the black African patients included in our sample, as LDL
hypercholesterolaemia is characteristically not very severe in
patients with diabetes. In addition, familial hypercholesterolaemia
is relatively common in Caucasian/European individuals, and
to a lesser extent in Asian South Africans, due to founder
effects. Achieving LDL-C goals in patients with familial
hypercholesterolaemia is more difficult, owing to very high
baseline LDL-C values.
A very low proportion of patients attained their LDL-C goal
when treated by a cardiologist or lipidologist. This may be due to
the higher proportion of patients with severe dyslipidaemia, such
as familial hypercholesterolaemia, managed by these specialities.
Patients with familial hypercholesterolaemia are unlikely to
reach LDL-C goal with LMTs that are currently available in
South Africa, and novel agents, such as PCSK9 inhibitors, would
be required to manage these patients.
Limitations
This study was subject to limitations that may influence its
findings. The study population is not fully representative of all
patients treated with LMT in South Africa. The participants
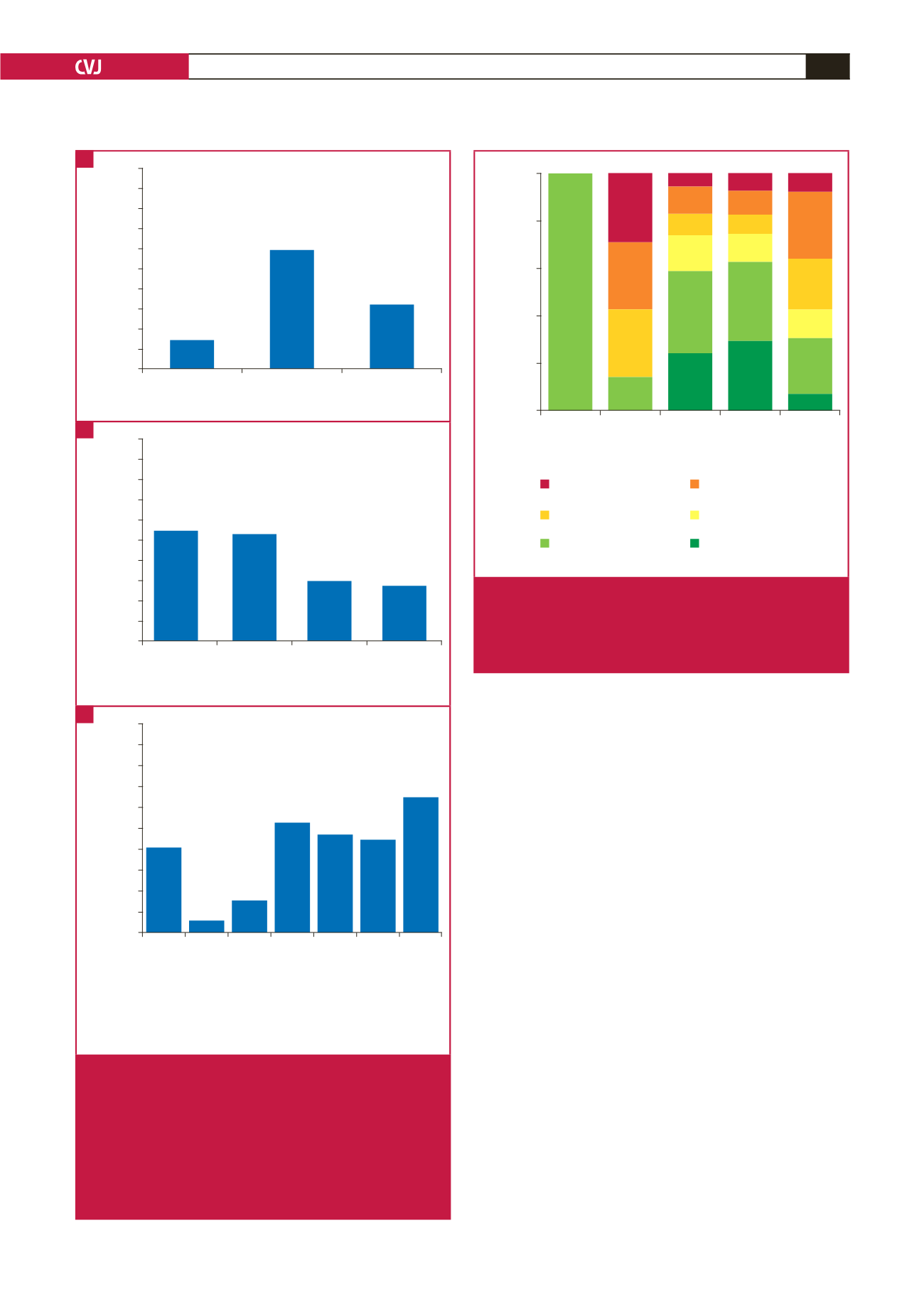
Calculated cardiovascular risk level (SCORE)
Low
(
n
=
1)
Moderate
(
n
=
7)
High
(
n
=
123)
Very high
(
n
=
223)
Not
assessable
(
n
=
42)
Patients within each LDL-C level category
at enrolment (%)
100
80
60
40
20
0
≥
1.8 to
<
2.6 mmol/l
(70–100 mg/dl)
<
1.8 mmol/l
(70 mg/dl)
≥
2.6 to
<
3.0 mmol/l
(100–115 mg/dl)
100
28.6
4.9
11.4
8.9
15.4
35.0
24.4
29.6
33.6
11.7
8.1
10.3
6.7
7.1
28.6
21.4
11.9
23.8
7.1
28.6
28.6
14.3
≥
3.4 to
<
4.1 mmol/l
(130–160 mg/dl)
≥
3.0 to
<
3.4 mmol/l
(115–130 mg/dl)
≥
4.1 mmol/l
(160 mg/dl)
Fig. 4.
Percentage of patients in each LDL-C value category
at enrolment (on lipid-modifying treatment), according
to calculated cardiovascular risk level (calculated using
SCORE
16
). LDL-C: low-density lipoprotein cholesterol;
SCORE: Systemic Coronary Risk Estimation.
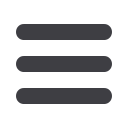
Patient’s cardiovascular risk level
Moderate risk
(
n
=
7)
High risk
(
n
=
123)
Very high
(
n
=
223)
Proportion of patients achieving
LDL-C goal (%)
100
90
80
70
60
50
40
30
20
10
0
14.3
59.3
32.3
Patient’s ethnicity
Asian
(
n
=
95)
Black African
(
n
=
79)
Caucasian
European
(
n
=
124)
Other
(
n
=
55)
Proportion of patients achieving
LDL-C goal (%)
100
90
80
70
60
50
40
30
20
10
0
54.7
53.2
29.8
27.3
Speciality of treating physician*
General practitioner
(
n
=
193)
Cardiologist
(
n
=
16)
Lipidologist
(
n
=
20)
Endocrinologist
(
n
=
40)
Internal medicine
(
n
=
19)
Other
(
n
=
45)
Several specialities
(
n
=
20)
Proportion of patients achieving
LDL-C goal (%)
100
90
80
70
60
50
40
30
20
10
0
40.9
6.3
15.0
52.5 47.4 44.4
65.0
Fig. 3.
Patients who achieved the 2011 ESC/EAS LDL-C
goals at enrolment,
5
according to (A) calculated
cardiovascular risk level (calculated using SCORE
16
),
(B) ethnicity, and (C) speciality of physician. EAS:
European Atherosclerosis Society; ESC: European
Society of Cardiology; LDL-C: low-density lipopro-
tein cholesterol; SCORE: Systemic Coronary Risk
Estimation. *
n
refers to the number of patients not the
number of physicians.
A
B
C

















