CARDIOVASCULAR JOURNAL OF AFRICA • Volume 26, No 2, March/April 2015
AFRICA
e5
findings, which was compression of the left common iliac vein by
the left common iliac artery. However, in surgery, it was seen that
it was a usual manifestation of MTS, which was a compression
by the right common iliac artery.
There are conflicting ideas about the usefulness of MRV for
the diagnosis of MTS. While Wolpert
et al
. reported that MRV
is the best modality for the diagnosis of MTS, McDermott
el
al
. suggested that MRV alone may not be sufficient to confirm
the diagnosis and could possibly lead to further investigation.
3,7
The disadvantage of MRV is that the vascular regions above
the bifurcations disturb non-laminar flow and can present
a confusing picture.
8
Although it showed misleading images
on compression of the left iliac vein, MRV was successful in
diagnosing MTS in our patient.
MTS is not a rare cause of venous abnormalities in the left
lower extremity. The incidence of MTS in patients with left lower
extremity swelling was found to be 37.5% out of 24 patients
detected by MRV.
3
However, it is not always symptomatic. Kibbe
et al
. reported that iliac vein compression is a frequent anatomical
variant in asymptomatic individuals, and may represent the
normal anatomical pattern. They demonstrated that 24% of 50
asymptomatic subjects had more than 50% compression of the
left common iliac vein.
9
Different surgical approaches for the treatment of MTS
include vein-patch angioplasty with excision of the intraluminal
bands, division of the right common iliac artery and relocation
behind the left common iliac vein or inferior vena cava, and
saphenous vein graft bypass to the inferior vena cava or
ipsilateral common femoral vein.
10
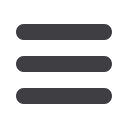
Saphenous graft bypass to
the inferior vena cava was performed on our patient, which was
successful in improving the symptoms.
Endovascular stenting of the iliac vein is another option in
the treatment of MTS. However, in young patients with difficult
anatomical variations, this may not be appropriate. Radiological
and surgical mismatch has been mentioned in our case. The
vascular surgery team also deals with endovascular treatment
modalities and they are experienced in these treatment options.
Stenting of the iliac vein in such a young patient may result in
early thrombosis of the stent. Therefore, we believe that surgical
correction of the pathological anatomy was the best option in
this case.
There are many reports in the literature discussing the results
of MTS with endovascular treatment. Thrombosed cases can
be treated with endovascular techniques. During endovascular
treatment, removal of the thrombi and then stenting the
compressed iliac vein segment can be done simultaneously.
9,11,12
The presented case was symptomatic but did not have deep-vein
thrombosis.
Conclusion
MTS should be taken into account in patients presenting with
swelling of the left lower extremity. Our case demonstrated
inconsistent findings between MRV imaging and surgery. A
surgeon should be available for such unexpected conditions.
References
1.
Mc Murrich JP. The occurrence of congenital adhesions in the common
iliac veins, and their relation to thrombosis of the femoral and iliac
veins.
Am J Med Sci
1908;
135
: 342–345.
2.
May R, Thurner J. The cause of the predominantly sinistral occurrence
of thrombosis of the pelvic veins.
Angiology
1957;
8
: 419–427.
3.
Wolpert LM, Rahmani O, Stein B,
et al
. Magnetic resonance venogra-
phy in the diagnosis and management of May-Thurner syndrome.
Vasc
Endovasc Surg
2002;
36
: 51–57.
4.
Fretz V, Binkert CA. Compression of the inferior vena cava by the
right iliac artery: a rare variant of May-Thurner syndrome.
Cardiovasc
Intervent Radiol
2010;
33
: 1060–1063.
5.
Dheer S,
Joseph AE, Drooz A.Retroperitoneal hematoma caused by a
ruptured pelvic varix in a patient with iliac vein compression syndrome.
J Vasc Interv Radiol2003;
14
: 387–390.
6.
Molloy S,
Jacob S,
Buckenham T,
et al
. Arterial compression of the
right common iliac vein; an unusual anatomical variant.
Cardiovasc Surg2002;
10
: 291–292.
7.
McDermott S,
Oliveira G, Ergül E,
et al
. May–Thurner syndrome: can
it be diagnosed by a single MR venography study?
Diagn Interv Radiol2013;
19
: 44–48.
8.
Evans AJ,
Sostman HD,
Knelson MH,et al
. 1992 ARRS Executive
Council Award. Detection of deep venous thrombosis: prospective
comparison of MR imaging with contrast venography.
Am J Roentgenol1993;
161
: 131–139.
9.
Kibbe MR, Ujiki M, Goodwin AL,
et al
.
Iliac vein compression in an asymptomatic patient population.J Vasc Surg
2004;
39
: 937–943.
10. Duran C, Rohatgi S, Wake N,
et al
. May-Turner syndrome: a case
report.
E Afr J Med
2011;
43
: 129–131.
11. Popat RA, Sze DY, Kuo WT,
et al
. Common iliac vein stenosis and risk
of symptomatic pulmonary embolism: an inverse correlation.
J Vasc
Interv Radiol
2011;
22
: 133–141.
12. Wang Y, Zhang X, Yu W,
et al
. Endovascular treatment of acute
proximal deep venous thrombosis secondary to iliac vein compression
syndrome: a novel technique for thrombus removal.
Chin Med J
2013;
126
: 3184–3186.
Fig. 4.
Postoperative image showing saphenous vein graft
between the left common iliac vein and the inferior
vena cava. SFV, saphenous vein.

















