CARDIOVASCULAR JOURNAL OF AFRICA • Volume 30, No 3, May/June 2019
AFRICA
185
<
130/80 mmHg. The current SAHS definition of hypertension is
shown in Table 3 for comparison.
What was the rationale for the changes?
It is reasonable to assume that the recommendations were based
largely on the SPRINT study.
9
In brief, the SPRINT study enrolled
hypertensive patients over 50 years, with a systolic BP between 130
and 180 mmHg, with clinical or subclinical CV disease without
diabetes or stroke, but including those with chronic kidney
disease. Patients were randomised to intense control of systolic
BP (
<
120 mmHg) versus usual control (
<
140 mmHg). The study
was stopped prematurely because in the intensive arm there was
significant reduction in major adverse CV events (MACE) [hazard
ratio (HR) 0.75 (0.64–0.89),
p
<
0.001], CV mortality [HR 0.57
(0.38–0.85),
p
=
0.005] and heart failure [HR 0.62 (0.45–0.84),
p
=
0.002].
As a result of the study, the new Canadian hypertension
guidelines recommended a target of
<
120/80 mmHg in those
patients meeting the SPRINT entry criteria.
10
However the
AHA/ACC recommended a target BP of
<
130/80 mmHg for
all hypertensives.
8
The slightly higher target was presumably
recommended as analysis of the results of SPRINT showed that
in weighing risks versus benefits, the best results were achieved at
a systolic BP of
<
132 mmHg.
9
What are the controversies?
Several controversies arose from these recommendations, but
central to this was the redefinition of hypertension and the
resultant changes in target. Although there is a clear relationship
between increasing BP and CV events, starting at 115/75 mmHg,
11
the definition of hypertension has been generally defined as
>
140/90 mmHg, based on a pragmatic definition where diagnosis
and treatment do more good than harm, as proposed by Rose.
12
The European hypertension guidelines of 2018 have not changed
the definition of hypertension,
10
and it is difficult to understand
how two authoritative guideline committees come to different
recommendations based on the same evidence.
13
There is currently no evidence to support treating patients
with systolic BP levels between 130 and 140 mmHg, without
additional markers of CV risk, to a target BP
<
130/80 mmHg.
This is highlighted in the ACC/AHA guidelines where there
was only a recommendation to treat low-risk hypertensives
pharmacologically at systolic BP levels between 130 and 140
mmHg.
8
The evidence from other studies involving high-risk patients
with previous stroke and diabetes (excluded from SPRINT)
was also not conclusive in finding benefit from intensive BP
control. In the ACCORD study, which was a similar study
to SPRINT and performed in high-risk patients with type 2
diabetes, intensive control of systolic BP (
<
120 vs
<
140 mmHg)
did not result in a significant reduction in MACE.
14
Therefore,
in contrast to the ACC/AHA guidelines, the American Diabetes
Association recommendation for the definition of hypertension
for diabetics remains unchanged at 140/90 mmHg, and most
patients with diabetes and hypertension should be treated to
a systolic BP goal of
<
140 mmHg and a diastolic BP goal of
<
90 mmHg. Lower systolic and diastolic blood pressure targets,
such as 130/80 mmHg, may be appropriate for individuals at
high risk of CV disease, if they can be achieved without undue
treatment burden.
15
Similarly, in the SPS3 study done in patients
with hypertensive stroke, intensive BP control did not meet the
primary end-point of reduction in stroke events, although there
was a significant reduction in incidence of haemorrhagic stroke.
16
Another controversy arising fromSPRINTwas the way the BP
was measured. This was done by automated devices and a mean
of three readings were taken that were generally unobserved. This
method of BP measurement is termed automated office blood
pressure (AOBP). It more accurately reflects daytime ambulatory
BP by reducing the white-coat effect and correlates better with
target-organ damage than conventional office BP.
17
Office systolic
BP in the standard clinical setting is on average 15 mmHg higher
than AOBP, presumably due to reduction in white-coat effect
and inaccuracies in standard office measurements.
18
Although
the improvement in accuracy of BP measurement in clinical
trials and practice is desirable, the lack of standardisation of
measurement between trials complicates the recommendations
ont targets and definitions of hypertension.
Important adverse events were reported in SPRINT and
ACCORD in the intensive group, mostly attributed to too-low
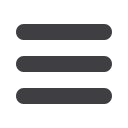
Table 2. BP targets according to the AHA/ACC hypertension guidelines (adapted reference 8)
Level of recommendation BP goal for patients with hypertension
I
For adults with confirmed hypertension and known CVD or ASCVD event risk
>
10%, a BP target
<
130/80 mmHg is recommended
IIb
For adults with confirmed hypertension without additional markers of increased CVD risk, a BP target
<
130/80 mmHg may be reasonable
CVD, cardiovascular disease; ASCVD, atherosclerotic cardiovascular disease.
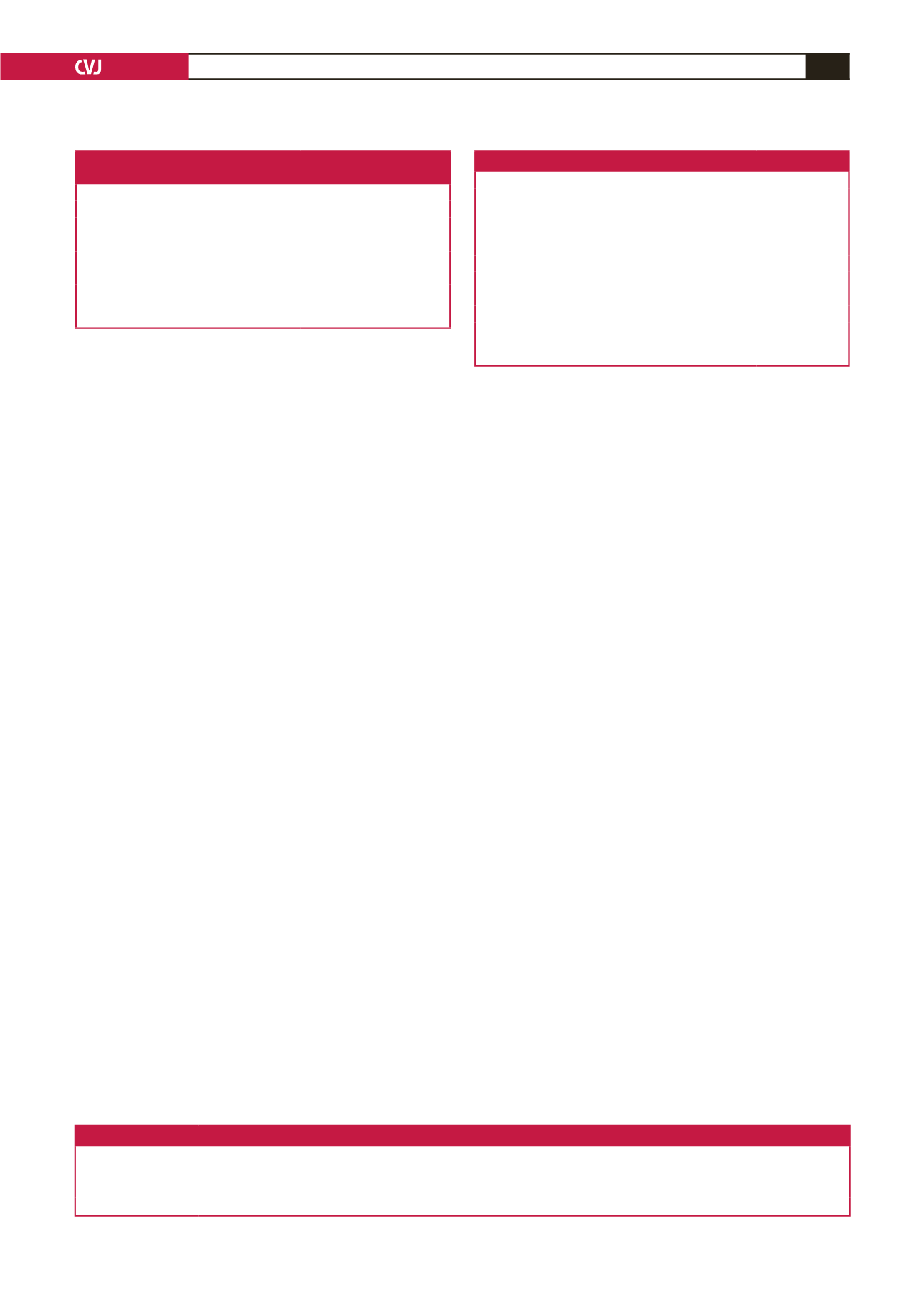
Table 3. Current SAHS definition of hypertension (adapted reference 1)
BP category*
SBP
DBP
Normal
<
120
and
<
80
Optimal
120–129
and
<
80
High normal
130–139
or
80–89
Hypertension
Grade 1
140–159
or
90–99
Grade 2
160–179
or
100–109
Grade 3
≥ 180
or
≥ 110
Isolated systolic
≥ 140
and
<
90
*Individuals with SBP and DBP in two categories should be designated to
higher BP based on two or more careful readings obtained on two or more
occasions.
Table 1. Classification of hypertension according to the AHA/ACC
hypertension guidelines (adapted reference 8)
BP category*
SBP
DBP
Normal
<
120
and
<
80
Elevated
120–129
and
<
80
Hypertension
Stage 1
130–139
or
80–89
Stage 2
≥ 140
or
≥ 90
*Individuals with SBP and DBP in two categories should be designated to
higher BP based on two or more careful readings obtained on two or more
occasions.

















