CARDIOVASCULAR JOURNAL OF AFRICA • Volume 29, No 4, July/August 2018
AFRICA
209
Submitted 15/10/16, accepted 14/1/18
Published online 8/12/17
Cardiovasc J Afr
2018;
29
: 208–212
www.cvja.co.zaDOI: 10.5830/CVJA-2018-007
Pulmonary hypertension (PH) is defined as an increase in mean
pulmonary arterial pressure (mPAP) at or above 25 mmHg at
rest.
1,2
It is currently classified by the World Health Organisation
(WHO) into five subtypes, which include pulmonary arterial
hypertension (PAH), PH due to left heart disease (PHLHD),
PH due to lung disease or hypoxia (PHLDH), chronic
thromboembolic PH (CTEPH) and PH due to unclear or
multifactorial mechanisms (PHUM).
3,4
The prevalence of pulmonary vascular disease in the
developing world is unknown, but estimates suggest that about
25 million individuals may be affected.
5
Little information exists
on the epidemiology of PH in sub-Saharan Africa, however
there is some evidence that based on the high prevalence of risk
factors such as rheumatic heart disease, schistosomiasis and HIV
infection in this area of the world, the prevalence and mortality
rate of PH may be higher than in Western countries.
6,7
In South Africa, PH has been identified as one of the
commonest causes of death, accounting for 31% of total
cardiovascular deaths,
8
while only 8% of cardiovascular
deaths in the United Kingdom were attributed to PH in 2012.
9
Furthermore, studies from the United States have shown that
the prevalence of PH among African Americans is higher than
in Caucasians.
10
These differences in the epidemiology of PH
in different regions of the world are determined by genetic,
geographic, environmental and socio-economic factors.
Left heart disease has been widely suggested to be the
most common cause of PH. In developing countries, chronic
infectious diseases, hypertensive heart diseases, cardiomyopathy
and rheumatic heart disease are the main contributors.
6
This
study aimed at determining the prevalence, baseline clinical
characteristics and mortality rate during six months of follow up
of patients with PH diagnosed via echocardiography at the rural
Shisong Cardiac Centre (SCC) in Cameroon.
Methods
This was a prospective cohort study in a sub-sample of 150
participants aged 18 years and older who were diagnosed with PH
via echocardiography. It was conducted at the Shisong Cardiac
Centre from September 2013 to December 2014. This study also
forms part of the Pan-African Pulmonary Hypertension Cohort
study (PAPUCO).
Shisong is a rural village in the Kumbo sub-division of the
north-west region of Cameroon. Shisong, on the outskirts of
Kumbo town, is about 400 km north of Douala, the economic
capital of Cameroon, and 450 km north-west of Yaoundé,
the political capital of Cameroon.
11
The Shisong Cardiac
Centre (SCC) is a well-equipped centre for the diagnosis and
management of a variety of cardio-surgical conditions including
PH. On average 185 echocardiographic examinations are done
per month. In this study, the target population was restricted
to patients living in rural or sub-urban areas, aged 18 years and
above, who underwent echocardiographic examination at the
centre between September 2013 and December 2014.
The PAPUCO study design and procedures have been
described in detail elsewhere.
12
In brief, PH was diagnosed
using echocardiography in patients with a right ventricular
systolic pressure (RVSP)
≥
35 mmHg in the absence of acute
right heart failure (HF) and pulmonary stenosis. The data-
collection form, adapted from the PAPUCO study, was used
to obtain patients’ information and clinical characteristics,
including socio-demographic factors and past medical history
[age, gender, body mass index (BMI), HIV status, family history
of cardiovascular disease, systemic hypertension, dyslipidaemia,
smoking and alcohol consumption], clinical presentation
(dyspnoea, cough, fatigue, pedal oedema, palpitations and
World Health Organisation functional classification).
At six months post-baseline, patients and/or their next-of-kin
were contacted by phone to determine their vital status. For all
fatal outcomes, the probable cause of death was assessed through
a verbal autopsy.
Statistical analysis
Data were analysed using SPSS
®
(Statistical Package for
Social Sciences for Windows) version 20. Qualitative variables
are summarised as frequencies and percentages. Continuous
variables are represented as means and standard deviations,
or median (25th to 75th percentiles). Patients were categorised
in three groups depending on PH severity; mild if RVSP was
36–50 mmHg, moderate if RVSP was 51– 60 mmHg and severe
if RVSP was
>
60 mmHg. We used
χ
² to compare proportions
and Student’s
t
-test or Kruskal–Wallis test to compare mean
differences for continuous variables. Statistical significance was
accepted at a
p
-value of 0.05.
Results
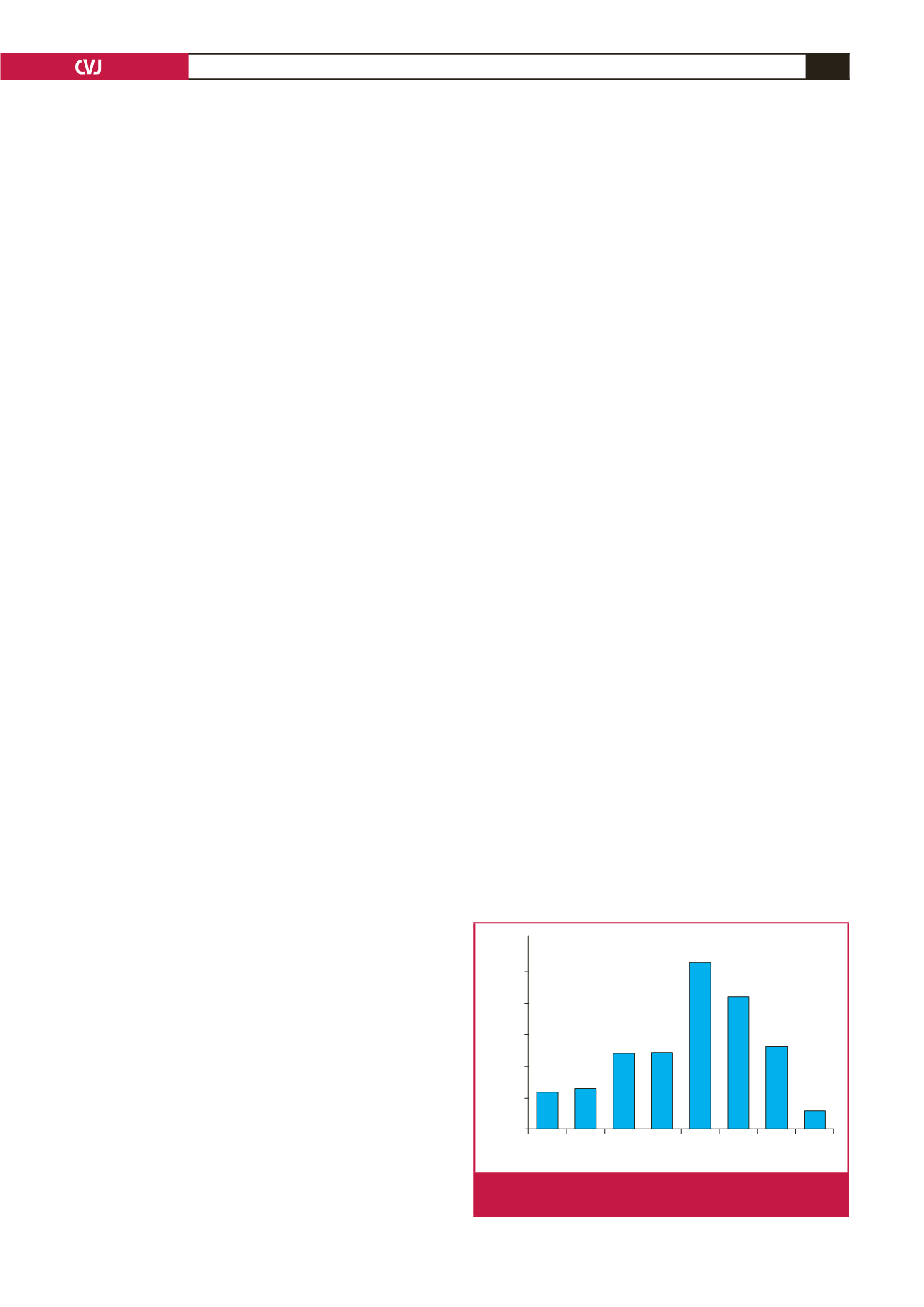
Out of a total of 2 194 patients who underwent cardiac
echography at baseline, 343 had PH (prevalence rate 15.6%).
Mean age was 61.9
±
18.0 years and female gender (189, 55.1%)
was predominant. As shown in Fig. 1, the peak prevalence of PH
was noticed between 60 and 69 years (91/343, 26.5%).
Characteristics of the sub-sample followed up (
n
=
150) were
similar to those of the overall PH group. The mean baseline age
was 62.7 years [standard deviation (SD)
=
18.7]. Mean age did not
Age group of patients with PH (years)
18–29 30–39 40–49 50–59 60–69 70–79 80–89 ≥90
Percentages
30
25
20
15
10
5
0
n
=
343
5.8 6.4
12.0 12.2
26.5
21.0
13.1
2.9
Fig. 1.
Age distribution of patients with pulmonary hyperten-
sion in the Shisong Cardiac Centre.

















