CARDIOVASCULAR JOURNAL OF AFRICA • Vol 23, No 3, April 2012
e10
AFRICA
abnormality in the LAD territory and the ejection fraction was
34%. The patient was loaded with 600 mg of clopidogrel and 325
mg of aspirin and was taken up for primary PCI.
The left coronary angiogram with a 6 Fr JL 3.5 guiding
catheter (Medtronic, Inc. Minneapolis, MN) showed a totally
occluded LAD at the proximal end of the stent (Fig. 1).
The lesion was easily crossed with a 0.14˝ Balance Middle
Wight universal guide-wire (Abbott Vascular, Santa Clara, CA).
Intravenous eptifibatide was started.
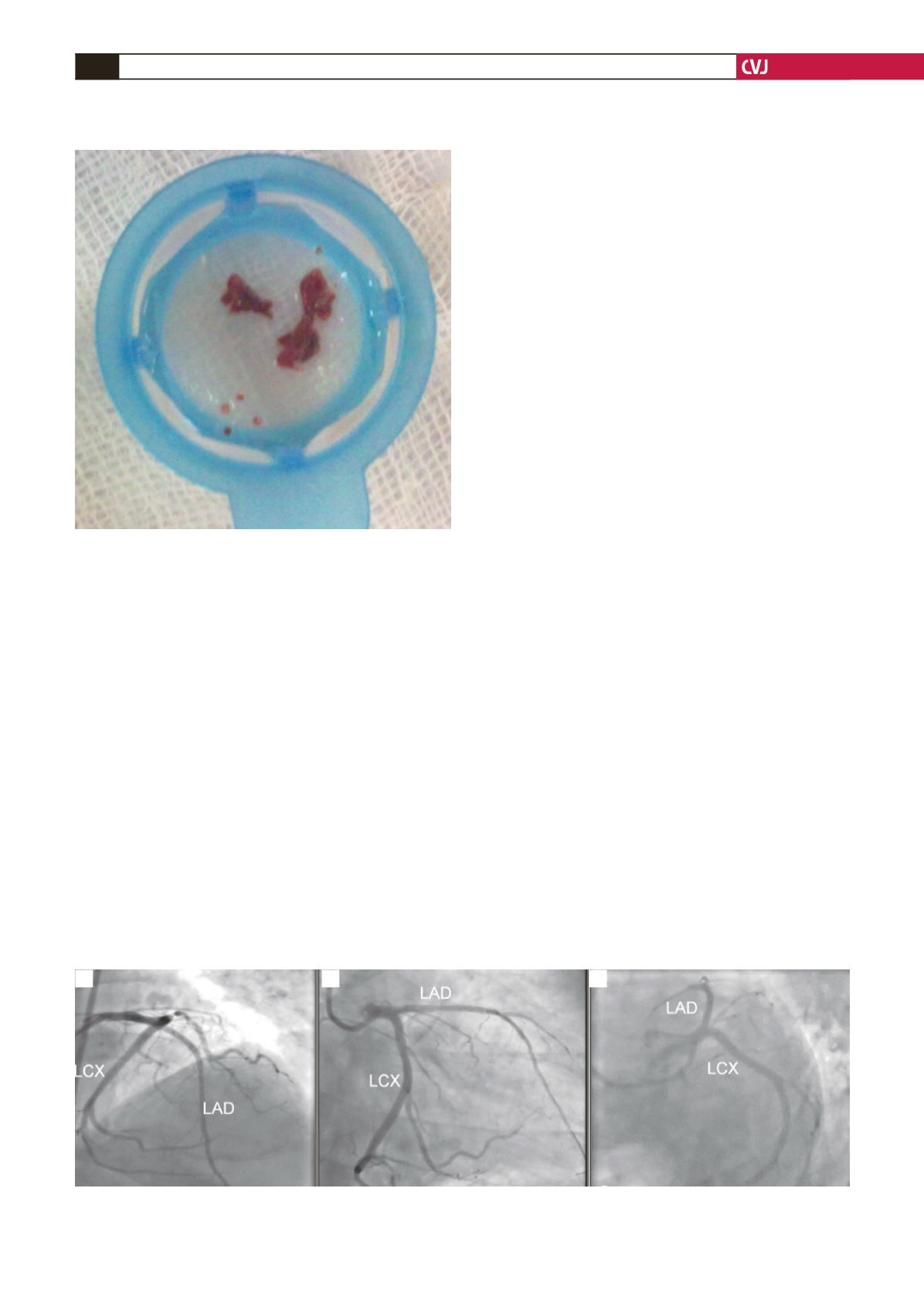
Thrombosuction was done with a 6 Fr Export XT catheter
(Medtronic, Inc, Minneapolis, Minnesota), which recovered
a substantial amount of thrombus (Fig. 2) and established
thrombolysis in myocardial infarction TIMI-3 distal flow with
minimal haziness at the proximal end of the stent. The stent
segment was dilated serially with a 3
×
10-mm Sprinter balloon
catheter (Medtronic, Inc, Minneapolis, Minnesota) at 9–10
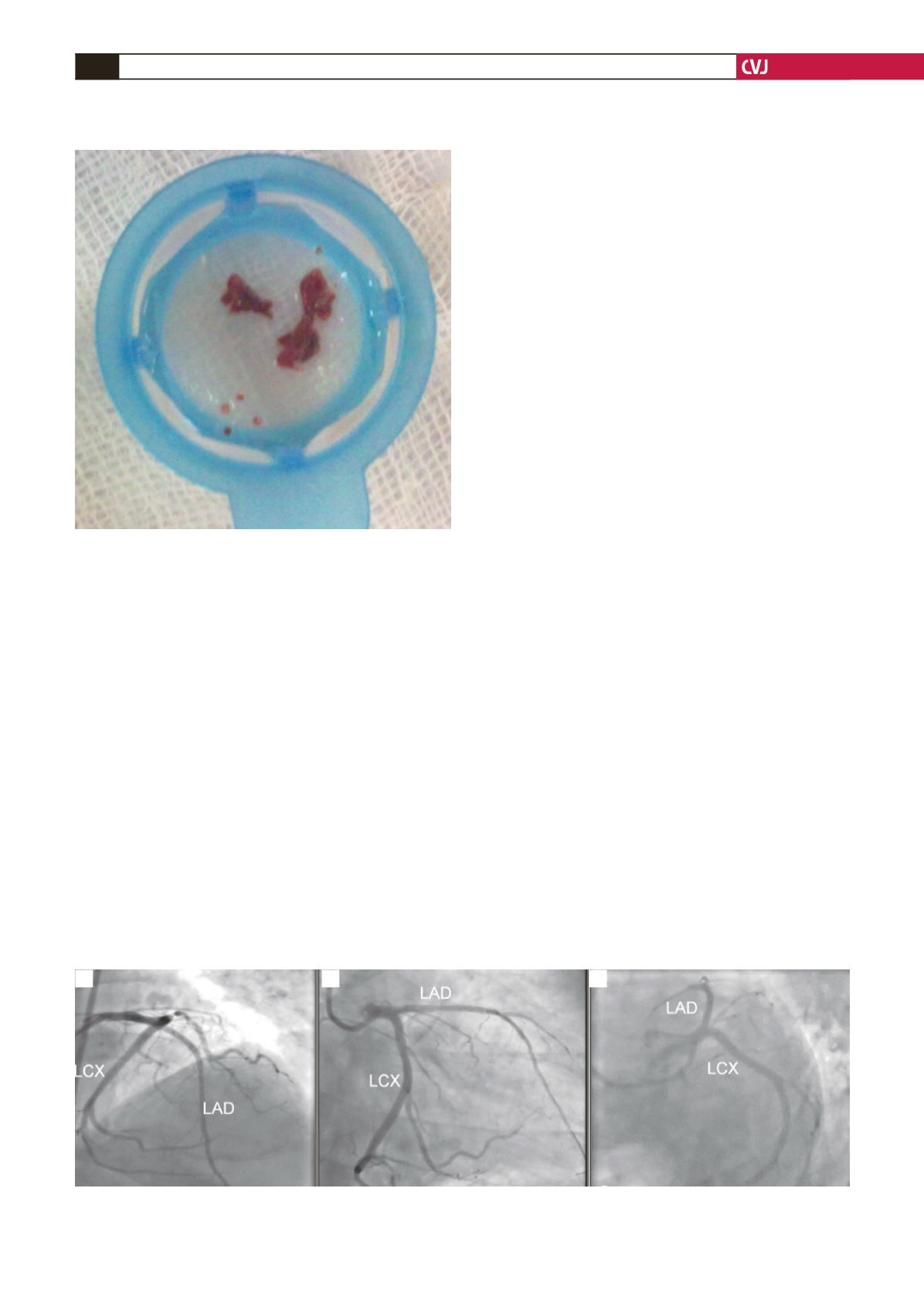
atmospheric pressure. The final angiogram showed TIMI-3 distal
flow (Fig. 3). The patient had good ST-segment resolution.
The peri-procedural period was uneventful. The patient
was discharged with dual anti-platelet treatment. He was
asymptomatic at one-year follow up.
Discussion
Late stent thrombosis occurs in 0.6% of patients following
DES implantation and is associated with increased mortality,
non-fatal myocardial infarction and the need for target-vessel
revascularisation.
2
DES thrombosis is a multi-factorial process
with impaired neo-intimal healing as the common denominator.
Other proposed mechanisms of stent thrombosis, from various
autopsy and imaging studies, are stenting across major arterial
side branches, incomplete stent expansion, stent mal-apposition,
stent fracture, long stent length, stent strut penetration of
the necrotic core, disruption of vulnerable plaque near the
stent, discontinuation of dual anti-platelet therapy, anti-platelet
resistance, radiation therapy and hypersensitivity vasculitis.
3
The process of neo-intimal healing, characterised by
development of an endothelialised layer of smooth muscle cells
and extracellular matrix completely covering the stent struts, is
delayed and incomplete after the implantation of drug-eluting
stents due to the inhibitory properties of the drugs. This has been
demonstrated repeatedly in autopsy and angioscopic studies.
3
In the angioscopic follow-up study byAwata
et al
., incomplete
neo-intimal covering with uncovered stent struts was seen
after two years, following sirolimus-eluting stent implantation,
whereas neo-intimal covering was complete with bare-metal
stents after six months. They also demonstrated yellow plaques
beneath the stent struts. However, none of their patients had stent
thrombosis as all were on dual anti-platelet therapy throughout
the period of follow up.
4
Chen
et al
., in their study on sirolimus-eluting stents with
optical coherence tomography (OCT), have shown similar
findings.
5
Velero
et al.
reported a case of stent thrombosis 53
months after sirolimus stent implantation. With OCT, they
reported uncovered stent struts with overlying thrombi after a
long period of time. They also showed lipid-rich plaque distal to
the stent border.
6
In our case, even though DES was implanted in the setting
of acute ST-elevation myocardial infarction, the procedure was
uneventful and the patient was asymptomatic for six years. The
patient continued to be on dual anti-platelet therapy until the
day of the event. The mechanism of stent thrombosis was not
clear in our patient. Intravascular ultrasound and OCT were not
performed due to unavailability. Focal thrombotic obstruction in
the vicinity of the proximal end of the stent may have been due
to unstable plaque rupture in this area.
Plaques covered with dysfunctional endothelium forming,
despite administration of an anti-mitotic drug and persistent
Fig. 2. Two pieces of aspirated thrombus using the
Export catheter.
Fig. 3. Final angiogram in the antero-posterior cranial (A), right anterior oblique caudal (B), and left anterior oblique
caudal (C) views, showing TIMI-3 distal flow.
A
B
C