CARDIOVASCULAR JOURNAL OF AFRICA • Volume 27, No 1, January/February 2016
e2
AFRICA
Two stents were implanted in the RCA and circumflex artery,
one after the other. Immediately after the procedure, the patient
developed chest pain. An emergency CAG did not identify any
culprit lesion.
Half an hour after the second CAG, the patient complained
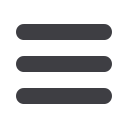
of severe chest pain. An ECG revealed ST-segment elevation in
leads V1–4, consistent with anteroseptal MI (Fig. 3B), which
had not been there before (Fig. 3A). The patient was taken
immediately to the catheterisation unit.
There was no occlusion in the implanted stents but the stent
in the RCA was under-expanded. Dilatation was performed,
however, the patient continued to experience chest pain.
Therefore, a stent was implanted for LAD stenosis. Initially, the
chest pain decreased but then increased again. A second stent
was deployed in the suspected dissection region in the LAD.
Echocardiography confirmed a structurally normal heart
with no obvious regional wall abnormality. An echocardiogram
revealed a localised apical pericardial effusion (Fig. 4).
The patient’s chest pain remained constant for several hours,
without any recurrence of elevated cardiac enzymes. His chest
pain was attributed to local pericardial irritation due to coronary
perforation by the guide wire during implantation of the stent
(Fig. 5).
Several days after the procedure, the ECG showed complete
resolution of the ST-segment elevation, with no pathological
Q wave (Fig. 3C). Given the combination of symptoms, ECG
changes and echocardiographic findings, a diagnosis of regional
pericarditis was made, despite the absence of a pericardial rub,
which is fleeting in nature.
Discussion
It is important for the clinician to differentiate acute MI/acute
stent thrombosis from pericarditis, which is a rare complication
of percutaneous coronary intervention. It can be difficult to
distinguish regional pericarditis from myocardial ischaemia with
ECG.
Echocardiography can be very useful in excluding regional
wall motion abnormalities and identifying pericardial effusion,
especially in atypical presentations of pericarditis. However, in
the acute setting, prompt differentiation of pericarditis from
myocardial injury by ECG remains of paramount importance to
avoid a delay in reperfusion.
Earlier reports confirm that it is frequently difficult to
differentiate between acute pericarditis and coronary occlusion.
3,4
The problem appears to be further confounded when
pericarditis is regional, with electrocardiographic features nearly
indistinguishable from localised MI, which could lead to the
incorrect treatment.
5
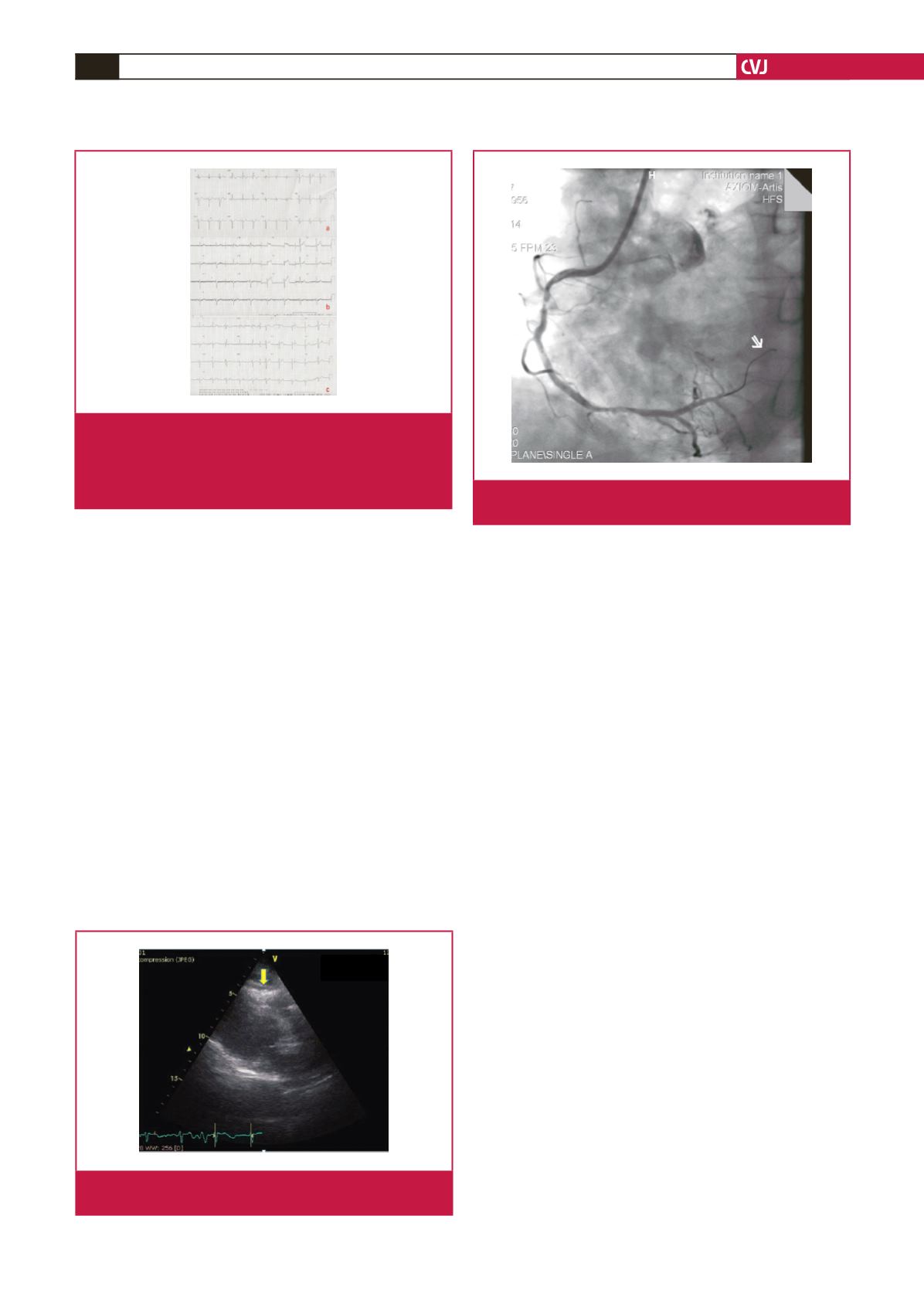
In this case, coronary perforation by the tip of the guide wire
most likely caused injury to the local pericardium,
6
as evidenced
by the anterior injury pattern that developed on the patient’s
ECG, mimicking MI. The complete resolution of the patient’s
ECG abnormalities, the absence of wall motion abnormalities,
and the lack of elevation of troponin I levels all support the
diagnosis of regional pericarditis.
Fig. 3.
A. ECG on hospital admission. B. Post-procedural ECG
shows ST-segment elevation in leads V1–4, consistent
with anteroseptal MI. C. Several days after the proce-
dure, the ECG showed complete resolution of the
ST-segment elevation, with no pathological Q wave.
Fig. 4.
The echocardiogram displayed a localised pericardial
effusion.
Fig. 5.
The guide wire was advanced too far in the distal part
of the right coronary artery during stent implantation.

















