CARDIOVASCULAR JOURNAL OF AFRICA • Volume 30, No 1, January/February 2019
AFRICA
e5
heparin, warfarin, fresh frozen plasma, and protein C and
protein S extract.
7
We present a case of a surgically treated
CTEPH patient with protein C and protein S deficiencies.
Case report
A 50-year-old female had been admitted to another university
hospital with exertional dyspnoea, palpitation and reduction in
effort capacity. She had been treated with medical therapy only
in that medical centre. Warfarin therapy had been started and
continued after discharge.
When she applied to our hospital, her effort capacity was
remarkably decreased, in New York Heart Association (NYHA)
functional class IV. She also had leg swelling and sometimes
haemoptysis. The patient was treated medically (bronchodilator
therapy, glycocorticosteroid, furosemide, nitroglycerin,
sildenafil) for severe dyspnoea and pulmonary hypertension in
our cardiology and chest disease clinics.
Because of the development of her symptoms, she was
referred to our clinic. Her weight was 65 kg and height was 165
cm. Blood pressure and pulse rate were in the normal range.
The second heart sound was increased and widely split on
chest auscultation. The lung sounds were normal. The liver was
detected 5 cm below the right costal margin. There was mild
bilateral leg oedema. The patient did not have any other risk
factors such as smoking history, hormone use and family history.
We did not find any thromboembolic focus for the pulmonary
embolism in our patient.
A biochemical study revealed that the patient’s protein C
activity was 34.9% (normal range: 70–150%) and protein S
activity was 22.7% (normal range: 65–160%). Her partial oxygen
pressure was 45 mmHg in room air on arterial blood gas analysis.
The cardiothoracic ratio was 55% on chest X-ray. Her left
ventricular ejection fraction was 60% and systolic PAP was 110
mmHg on echocardiography.
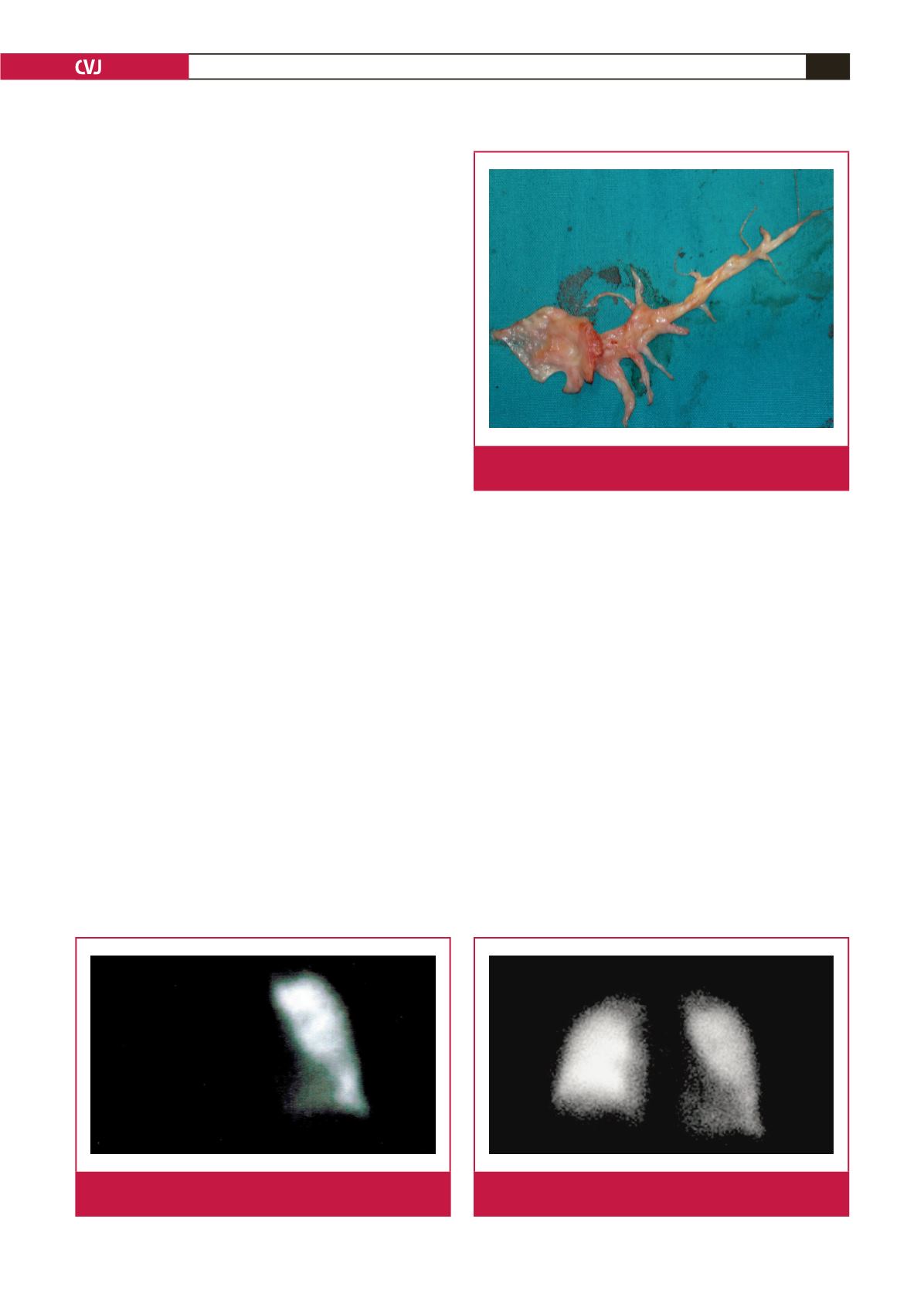
V/Q scan showed total occlusion of the right pulmonary
artery (Fig. 1). Cardiac catheterisation showed that the systolic
PAP was 110 mmHg and diastolic PAP was 9 mmHg (mean PAP
56 mmHg), right ventricular pressure was 110/0 mmHg (mean 25
mmHg), and pulmonary capillary wedge pressure was 10 mmHg.
The pulmonary angiogram showed total right pulmonary artery
occlusion. The patient was haemodynamically stable but urgent
surgery was planned because of low partial oxygen pressure and
severe clinical symptoms.
After a median sternotomy, cardiopulmonary bypass (CPB)
was established by cannulation of the aorta and two-stage
caval cannulation. The patient was cooled to 18°C, the aorta
was cross-clamped and cardiac arrest was established using
antegrade blood cardioplegia and local cold application. The
pulmonary arteries were explored by moving the aorta to the
right side.
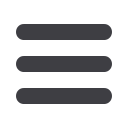
PEA was performed through right and left pulmonary
incisions under total circulatory arrest (TCA) (Fig. 2). Firstly, we
performed PEA on the right pulmonary artery and its branches
within 20 minutes. There after we performed a left pulmonary
artery incision for PEA in 12 minutes, but there were no
thromboembolic material in the left pulmonary artery. The TCA
time was 32 minutes and aortic cross-clamp time was 81 minutes.
Ultrafiltration was performed on the patient and about 2 500 cm
3
was filtered from the patient during CPB.
Alprostadil infusion and nitric oxide inhalation were
administered after surgery. Alprostadil infusion was administered
at a dose of 50 ng/kg/min for two days after the operation. Nitric
oxide inhalation therapy was maintained until the patient was
extubated at postoperative 18 hours. A low-molecular-weight
Fig. 2.
The pulmonary thromboendarterectomy material that
was removed from the right pulmonary artery.
Fig. 3.
There were no perfusion defects in the lungs on V/Q
scan after the operation.
Fig. 1.
Pre-operative total perfusion defect in the right lung
on V/Q scan.

















