CARDIOVASCULAR JOURNAL OF AFRICA • Volume 30, No 1, January/February 2019
AFRICA
65
Bernoulli’s equation then allows for the estimation of the RVSP,
12
taking into account right atrial pressure (RAP):
RVSP
=
TR MIG
+
RAP.
RAP is estimated from the inferior vena cava (IVC) calibre and
respiratory collapsibility (Table 1, Fig. 3B). In the absence of
pulmonary stenosis and acute right HF, the estimated RVSP is
assumed to equal the pulmonary artery systolic pressure.
To avoid errors in the measurement of RVSP, it is mandatory
to observe some conditions, including accurate measurement of
the IVC, avoiding measuring over-gained (shaggy) signals (Fig.
3A). If the heart rhythm is irregular, it is recommended that three
to five consecutive cycles be measured and the mean of these
cycles be recorded.
In patients with PH, Doppler echo also contributes to the
evaluation of the RV systolic function through measurement
of the tricuspid annular plane systolic excursion movement
(TAPSE). TAPSE represents the distance of systolic excursion of
the RV annular plane towards the apex. As shown in Fig. 3D, it is
obtained using an M-mode cursor passed through the tricuspid
lateral annulus in the four-chamber view and measuring the
amount of longitudinal displacement of the annulus at peak
systole.
In the PAPUCO registry,
11
Doppler echo findings showed that
left ventricular (LV) function was moderately impaired overall
(median LV ejection fraction 46%) (Fig. 3C). As expected,
RVSP was markedly elevated (median value 58 mmHg), with
concurrent moderate to severe right atrial (58%) and right
ventricular (55%) hypertrophy a common feature. Only one-third
of cases (
n
=
69; 33%) showed no evidence of right atrial or
ventricular enlargement. Overall, 78 patients (37%) presented
with a diagnosis of right HF based on TAPSE movement < 15
mm (Fig. 3D) plus one or more clinical signs of HF.
The LHD aetiology
13
of PH is suggested by (1) presence of
heart disease as suggested by a dilation in the cavities (Fig. 3E),
presence of heart valve disease or abnormal contractility, and (2)
arguments suggestive of an elevation of left ventricular filling
pressure, such as left atrial dilation (Fig. 3E) or a mitral Doppler
restrictive pattern (Fig. 3F). In the subgroup of patients with
PHLHD,
13
aetiologies were predominantly hypertensive HF with
reduced or preserved ejection fraction, dilated and peripartum
cardiomyopathy and rheumatic valvular heart disease. Left
atrium size and TAPSE were predictors of RVSP in these
patients, and RVSP predicted short-term hospitalisations but
not mortality.
We therefore recommend that an estimated RVSP greater
than 35 mmHg in SSA should warrant further evaluation for PH
in patients with suggestive PH in step 1 and/or 2 (Fig. 1). Finally,
Doppler echo can clearly help identify possible aetiologies
of PH, and particularly PHLHD (Table 2), anticipating the
contribution of other tests.
Step 4: other investigations
A careful selection of other tests can contribute to establishing
a diagnosis of PH in patients residing in low-income countries
such as SSA. The utilisation of these other investigations will
depend on both the results of the above initial tests and the
clinical context. Given the high burden of HIV/AIDS in the
region as well as its contribution in the PAPUCO registry
(22%), it is reasonable to screen all patients with PH for HIV.
Other tests, such as abdominal ultrasound, liver-function test,
high-resolution computerised tomography (CT), CT pulmonary
angiography, ventilation/perfusion lung scan, and electrophoresis
of haemoglobin will be guided by the clinical context. It is only
after these steps have been completed and once a definitive
diagnosis of PH has been reached and potential underlying
co-morbidities or causes identified, that classification within an
appropriate aetiological group must be considered (Fig. 4).
We acknowledge classification difficulties in SSA and other
low-income countries, especially in the absence of RHC and
Table 1. Estimation of right atrial pressure from inferior vena cava
calibre and respiratory collapsibility. Adapted from Beigel
et al
.
12
Estimated RAP (mmHg) IVC diameter (cm)
IVC collapse with
inspiration (sniff)
5
< 2.1
>
50%
10
< 2.1
< 50%
15
≥
2.1
>
50%
20
≥
2.1
< 50%
RAP, right atrial pressure; IVC, inferior vena cava.
Table 2. Possible causes of pulmonary hypertension identified by
echocardiography with relevance to sub-Saharan Africa
13
Predisposing conditions for pulmonary hypertension
• Valvular disease [mitral (aortic) stenosis/regurgitation, prosthetic valve
dysfunction]
• Left ventricular systolic dysfunction (including hypertensive heart failure,
dilated cardiomyopathy, peripartum cardiomyopathy, myocardial infarction)
• Left ventricular diastolic function (including ischaemic heart disease, hyper-
tensive heart disease, hypertrophic cardiomyopathy, Fabry’s disease, infiltra-
tive cardiomyopathies)
• Other obstructive lesions (coarctation, supravalvular aortic stenosis, sub-
aortic membrane, cor triatriatum)
• Congenital disease with shunt [atrial (ventricular) septal defect, coronary
fistula, patent ductus arteriosus, anomalous pulmonary venous return]
• Pulmonary embolus (thrombus in inferior vena cava, right-sided cardiac
chamber, or pulmonary artery; tricuspid or pulmonic valve vegetation)
• Pulmonary vein thrombosis/stenosis
Findings that suggest specific disease entity
• Left-sided valve changes (systemic lupus erythematous, anorexigen use)
• Intra-pulmonary shunts (hereditary haemorrhagic telangiectasia)
• Pericardial effusion (idiopathic pulmonary arterial hypertension, systemic
lupus erythematous, systemic sclerosis)
Group 3
PH due to lung
disease and/or
hypoxia.
e.g. COPD or
tuberculosis
Group 1
Pulmonary arterial
hypertension.
e.g. HIV-associated PH
Group 2
PH due to left heart disease.
e.g. mitral stenosis due to
rheumatic heart disease
Group 5
PH with unclear or
multifactorial mechanism.
e.g. endomyocardial fibrosis
Group 4
Chronic thromboembolic PH.
e.g. chronic pulmonary
embolism
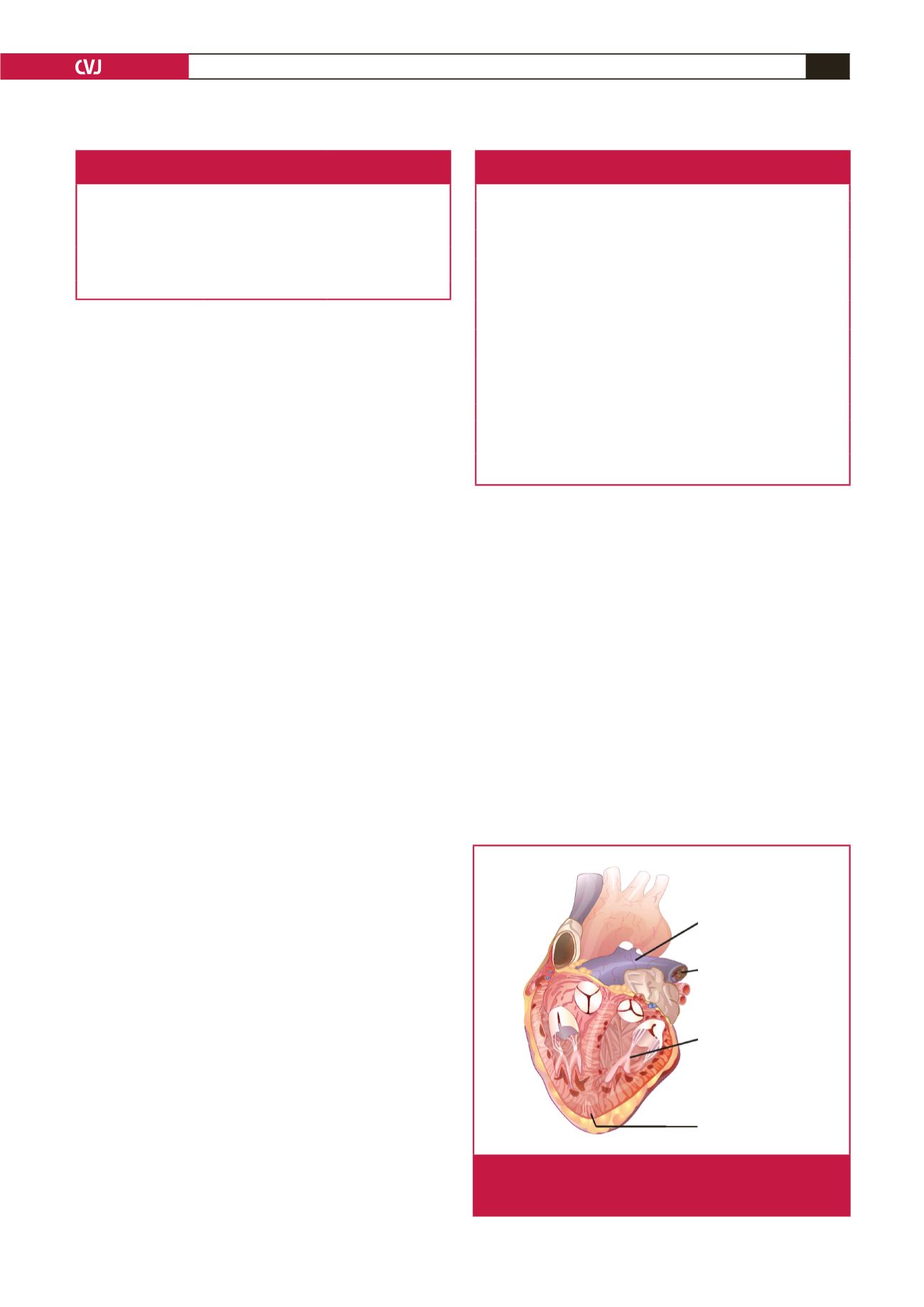
Fig. 4.
World Health Organisation classification of pulmonary
hypertension with relevant examples for sub-Saharan
Africa.
1

















